Table of Contents
Bone Quality vs Bone Density
The stronger your bones, the greater their ability to withstand fracture. However, what’s the best way to assess the strength of your bones? What do we mean when we compare bone quality vs bone density?
This article will answer these questions, discuss how we measure bone quality, provide guidelines on how to improve bone quality, and explore the relationship between bone quality and osteoporosis.
Bone Quality and Bone Density
The National Cancer Institute defines bone density as a “measure of the amount of minerals (mostly calcium and phosphorous) contained in a certain volume of bone.” The DEXA exam measures bone mineral density (BMD).
Health professionals use the BMD score to evaluate and classify bone health into one of several classes, including osteoporosis and osteopenia. Bone mineral density (BMD) tests are generally easily accessible, inexpensive, and safe. Later in this post, we describe the advantages and shortcomings of using bone density to evaluate bone health.
Bone quality refers to the material properties and architecture of the bone. It has to do with how bone is made, the cortical margin, the fabric of the trabeculae inside the bone, and porosities in the cortical part. A bone with “higher quality” is better able to withstand stress and potentially fracture. There are several ways to measure bone quality. We discuss these options later in this post.
In general, bone quality is a better way to evaluate bone health compared to bone density.
Bone Density and Bone Health
Medical professionals often use bone density to assess bone health. They use Dual Energy X-ray Absorptiometry (DEXA) that measures bone mineral density (BMD).
They frequently use this score to estimate your risk of fracture, select your best treatment options, and determine whether you should or should not take osteoporosis medication.
However, it has been known for over a decade that the DEXA test is not as reliable a measure of bone strength as originally thought. (1)
Bone Mineral Density (BMD) and Fracture Risk
In fact, several studies have shown that many fractures occur in people with only moderately decreased bone mineral density. (2,3)
Further, half of all postmenopausal fractures occur in women with bone mineral density (BMD) test results that indicate that their bone density levels are not low enough for them to be categorized as having osteoporosis. (4)
In addition, the results of the BMD test often determine whether you end up on medication or not. The most popular osteoporosis medications, both bisphosphonates and Prolia, are frequently prescribed to increase the density of bone.
These medications increase bone density, but do not necessarily improve the quality of bone.
Bone Strength and Bone Health
In his review, Bone Quality: The Determinants of Bone Strength and Fragility (5), published in Sports Medicine in 2013, Dr. Helder Fonseca defines bone strength as “the maximal amount of load tolerated before structural failure occurs.”
Dr. Helder explains the relationship between bone strength and the risk of fracture: “Failure gradually builds within the [bone] material as micro-cracks develop. Strains [eventually] reach an unbearable critical limit. Bone strength and toughness are therefore highly dependent on the ability of the bones to dissipate the stresses that lead to increases in strain, as well as on the micro-structural properties that prevent crack propagation.”
This explains why a vertebral compression fracture is the result of the buildup of small micro-cracks that develop over time and eventually lead to a fracture.
The next section throws light on how bone strength, and in particular, bone structure, influence frailty and eventually the chance of fractures. including compression fractures and femoral neck fractures.
Bone Strength and Fracture Risk
In 2016 Dr. Georg Osterhoff and colleagues published a report in the journal Injury, entitled Bone mechanical properties and changes with osteoporosis (6), that examined the relationship between bone quality and osteoporosis. Dr. Osterhoff reported several important findings.
Bone Fragility and DEXA
First, Dr. Osterhoff states: “The assessment of bone mineral density (BMD) as a surrogate marker of bone strength using non-invasive methods like dual-energy X-ray absorptiometry (DEXA) is widely regarded as the gold standard for diagnostic screening and as a guide prior to therapeutic decisions.
However, BMD accounts for only 60% of the variation in bone fragility because it is unable to depict differences in bone material composition and structural design. Both characteristics influence bone strength to a large extent.”
In other words, while DEXA evaluation of BMD is seen as the “gold standard,” it can only account for 60% of the measure of bone fragility. Bone fragility reflects the ability of your bones to resist fracture (discussed in more detail later in this post.)
As a result, you could receive a good BMD score, but there is still a risk of a fracture because the DEXA cannot evaluate “bone material composition and structural design,” or bone structure.
Bone Fragility and Movement Patterns
Second, Dr. Osterhoff notes that when we evaluate bone, we should consider its ability to withstand different movement patterns, such as rotation and lateral movements. He explains this here:
“The unique mechanical properties of bone reflect the need to provide at the same time strength and lightweight design, stiffness and elasticity, the ability to resist deformation, and the ability to absorb energy.”
These dynamic movements happen in everyday life when you exercise, work in your garden, pick up your grandchildren, or shop for groceries.
Bone is both strong and pliable. It is not a rigid structure.
Bone Fragility and Trabecular Connectivity
Third, Dr. Osterhoff reports that: “aging and other factors like estrogen deficiency can affect these components and eventually result in decreased bone strength and fracture toughness.”
He also states that “osteoporotic fractures are the macroscopic result of a sequence of multiple nano- and micro-structural events.”
The source of these osteoporotic fractures is the inability of our bones to withstand different types of loads.
Later in this post, we will talk about the different types of bone and their role in resisting fracture. However, at this time, I should point out that trabecular (also referred to as cancellous) bone composition plays a critical role in whether you experience a fracture or not.
Dr. Osterhoff states in his report that “trabecular connectivity inside a bone contributes more to the bone’s biomechanical strength than the trabecular thickness or the bone mineral density.”
Recent medical research demonstrates that good bone structure (or bone quality) is more important than the density of your bones when determining the strength of your bones (and their ability to resist fracture.)
Unfortunately, the BMD test or DEXA does not provide information on the quality of your bone or any insight into the architectural structure of your bones.
What is Bone Quality?
I asked Dr. Janet Rubin to define bone quality. Dr. Rubin is the Sarah Graham Kenan Distinguished Professor and Vice Chair for Research at the Department of Medicine of the University of North Carolina in Chapel Hill. She is also the Professor of Medicine in the Division of Endocrinology and Metabolism, a Joint Professor in Pediatrics and Pharmacology, and an Adjunct Professor for Bioengineering.
In the interview, Dr. Rubin explains that “bone quality is the architecture of the bone. It has to do with how bone is made, the cortical margin, the fabric of the trabeculae inside the bone, and porosities in the cortical part. Bone quality represents the material properties, where the materials are, and the architecture of the materials.”
Bone quality is an essential ingredient in bone structure and strength, as well as the bone’s ability to resist fracture. A major challenge is how to easily measure bone quality.
Dr. Helder explains in his paper (5) that “bone mineral density (BMD) is only able to provide insight regarding the quantity of bone tissue. It is insufficient as a measure of bone quality, given that bone strength is dependent on a large variety of interconnected factors.”
Bone Quality and Osteoporosis
To gain a better understanding of the relationship between bone quality and osteoporosis, we need to cover bone anatomy in some detail.
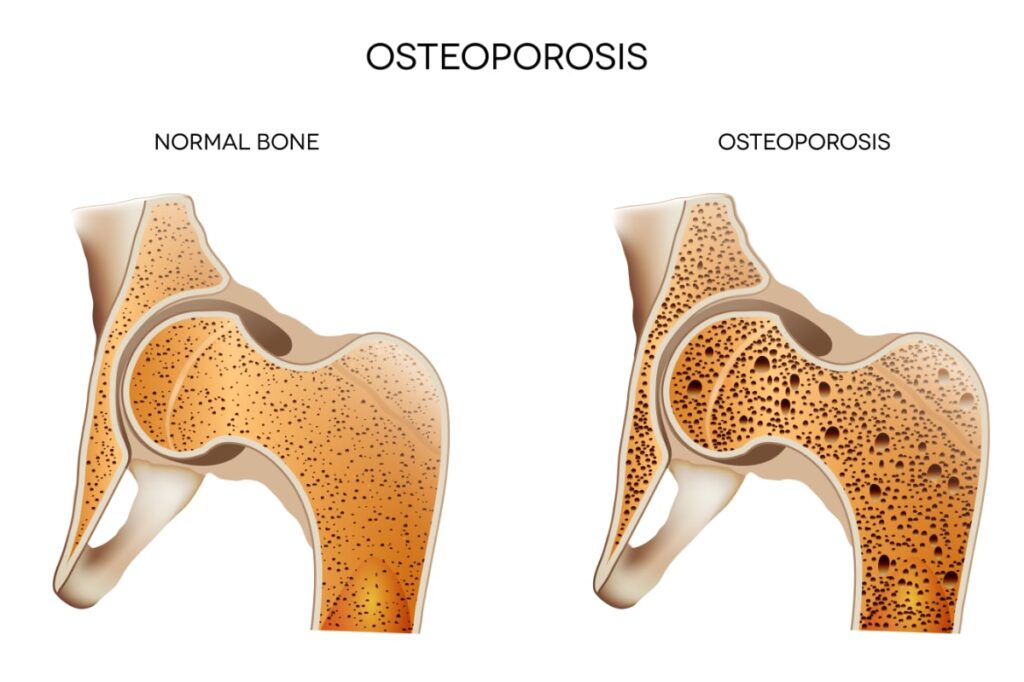
Bone tissue (or osseous tissue) refers to the bone. There are two types of bone tissue: cortical bone and cancellous (trabecular) bone.
An individual bone can be composed of both cortical and cancellous bone, and the relative mix of the two types varies from bone to bone in your body.
Cortical Bone
Cortical bone (sometimes referred to as compact bone) forms the cortex or outer shell of most bones. It is much denser, rigider, and stronger than the other type of bone tissue, cancellous bone.
Cancellous Bone
Cancellous bone (also referred to as trabecular or spongy bone) appears at the end of long bones, at the points of attachment of joints, and within the interior of the vertebrae. It has a greater surface area and is more porous, softer, less dense, and less stiff than cortical bone. As a result, cancellous bone is more affected by osteoporosis than cortical bone.
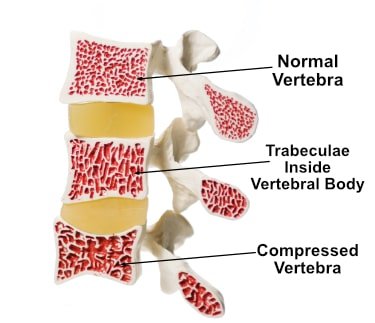
Bone Quality and Vertebral Body
Because the vertebral (spinal) area is largely composed of cancellous (trabecular) bone, it is at a greater risk of osteoporotic fracture when compared to other parts of the body.
The image to the right shows a cross-section of the vertebral body.
The vertebral body is the portion of the spinal column facing into the body. Note how the porous structure of the trabecular bone varies depending on the quality of the bone.
The vertebral body at the top of the spinal column is healthy. This is indicated by the dense trabecular bone.
The vertebral body at the bottom of the spinal column segment has been compressed (a compression fracture) because of the reduced trabecular bone. The bone quality in this case has been compromised.
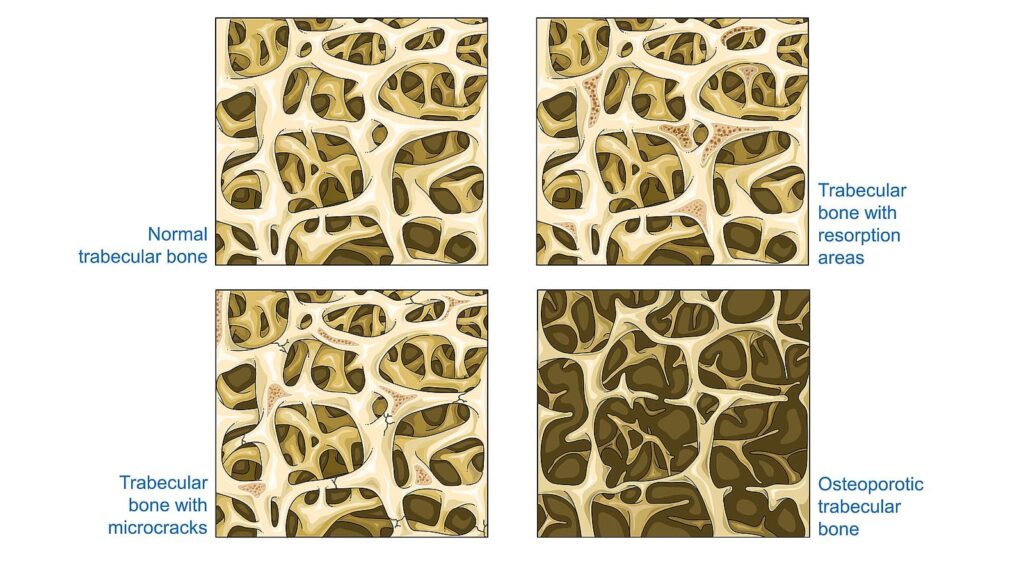
Cancellous bone is composed of many individual and interconnected trabecula.
Trabecula is a small, microscopic tissue element.
They look like beams (“trabecula” is Latin for “small beam”) and are often in the form of small rods or plates. The plural of trabecula is trabeculae.
What is the Trabeculae?
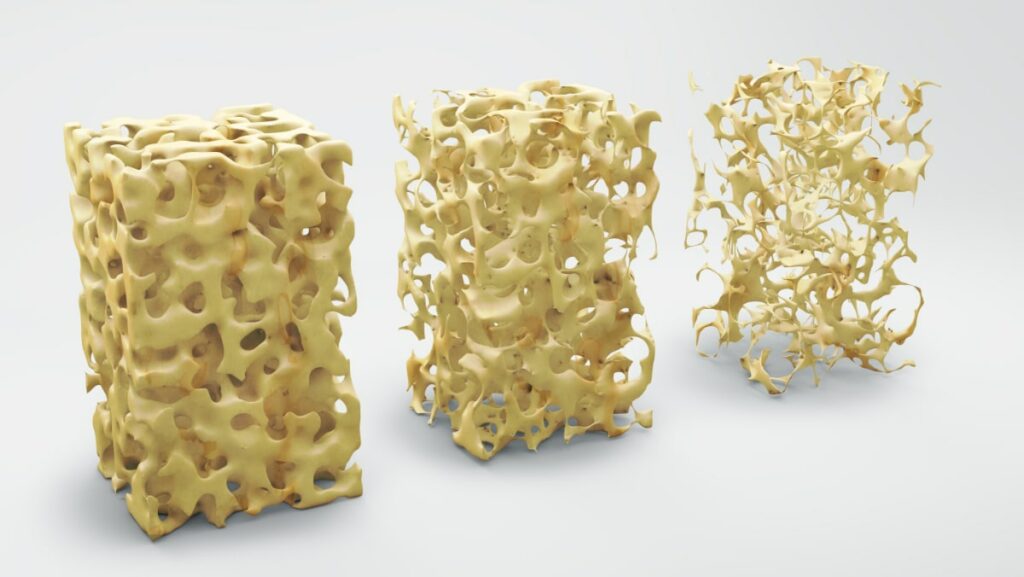
When we talk about bone quality and osteoporosis, we are specifically referring to the quality of the cancellous or trabecular bone. Bone quality is defined as the sum of the structural and material properties of the trabecular bone.
Think of trabecular bone as similar to the scaffolding that holds a building up.
A building composed of concrete is solid but rigid and inaccessible. Instead, the building should have support beams, struts, and strong interconnected pieces that allow the building to stand tall and flexible at the same time.
Either through ageing, disuse, or disease, the interconnected trabecular bone interconnections begin to break down. Even with anabolic therapy, it’s very rare that trabeculae reconnect. Although there may be a buildup of bone density, there can still be a loss of bone quality.
Trabecular Bone and Bone Structure
Bone structure is the composition of the trabecular bone inside the bone. Trabecular or cancellous bone is made up of many interconnected trabeculae, either in the shape of a rod or a plate.
The illustration above shows a microscopic view of a trabecular bone. Note the mix of flatter, plate-like trabecula interweaved with the narrower, rod-like trabecula in the top left of the image.
The more of the thicker plate-like trabeculae present in the structure as compared to the thinner, rod-like trabeculae, the better the quality of the bone.
The better the bone quality, the stronger the bone.
Trabecular Bone
Trabecular bone that has been replaced by rod-like trabecula is weaker, osteoporotic, and more at risk of a fracture. This change can occur over time and is dependent upon the individual’s family history as well as exercise and nutritional history.
Note the higher frequency of plate-like trabecula in the bone structure of the normal trabecular bone (top left of the image) when compared to the bone structure of the osteoporotic trabecular bone (bottom right of the image). In addition, the osteoporotic trabecular bone has more rod-like structures.
The material properties refer to substances or matter such as collagen and minerals that make up the bone.
Exercise Recommendations for Osteoporosis
Exercise is an essential ingredient to bone health. If you have osteoporosis, therapeutic exercise needs to be part of your osteoporosis treatment program.
But what exercises should you do and which ones should you avoid? What exercises build bone and which ones reduce your chance of a fracture? Is Yoga good for your bones? Who should you trust when it comes to exercises for osteoporosis?
A great resource on exercise and osteoporosis is my free, seven day email course called Exercise Recommendations for Osteoporosis. After you provide your email address, you will receive seven consecutive online educational videos on bone health — one lesson each day. You can look at the videos at anytime and as often as you like.

Topics Covered in Course
I cover important topics related to osteoporosis exercise including:
- Can exercise reverse osteoporosis?
- Stop the stoop — how to avoid kyphosis and rounded shoulders.
- Key components of an osteoporosis exercise program.
- Key principles of bone building.
- Exercises you should avoid if you have osteoporosis.
- Yoga and osteoporosis — should you practice yoga if you have osteoporosis?
- Core strength and osteoporosis — why is core strength important if you have osteoporosis?
Enter your email address and I will start you on this free course. I do not SPAM or share your email address (or any information) with third parties. You can unsubscribe from my mail list at any time.
Age, Bone Loss and Localized Fractures
Trabecular bone, due to its lesser density when compared to cortical bone, accounts for approximately 20% of the skeletal bone mass. However, trabecular bone is responsible for most of the bone turnover during the early stages of osteoporosis (in people under the age of 65).
As a result, Dr. Fonseca (5) states, “vertebral compression fractures, being ‘trabecular fractures’, are more common in individuals aged less than 65 years.”
Conversely, as we age, cortical bone becomes more and more porous and weaker. Dr. Fonseca notes that “with increasing cortical bone loss after the age of 65 years, hip fractures, being ‘cortical fractures’, become more frequent.”
Bone Location and Fracture Risk
Bone is subject to a number of forces as we move, specifically compressive and shearing loads.
In his paper (6), Dr. Osterhoff points out that “each bone’s location in the body and the forces acting on it determine its characteristic microstructure and composition.”
He points out that “vertebral bodies must resist high and repetitive axial compression loads.” Further, they “experience much less shear or tension loads. If the trabecular bone is reduced in a vertebral body, this leads to increased cortical shell stresses and a disproportionate decrease in the vertebral bone’s ability to withstand compression forces.”
In other words, if the trabecular struts within the vertebral body diminish, pressure is placed on the cortical bone to support the compressive forces through the spinal column.
“The femoral neck, on the other hand, is mainly subjected to shear forces and bending — the latter of which creates a combination of compression, tension, and shear.”
This makes intuitive sense. The hip area must support every day movements that include bending and squatting. As the bone quality diminishes in the femoral area, the risk of a femoral fracture increases correspondingly.
Bone Quality and History of Physical Activity
Your history of physical activity throughout your life can affect the quality of your bones in different locations.
In March 2020, Dr. Carrie Anne Ng (and colleagues) at Monash University published a paper (7) in the journal Osteoporosis International entitled Associations between physical activity and bone structure in older adults: does the use of self-reported versus objective assessments of physical activity influence the relationship?.
In the paper, Dr. Ng examined the effects of physical activity (during different periods) on bone locations. Dr. Ng stated: “In postmenopausal women with low bone mineral density (BMD), current physical activity (PA) was positively associated with femoral neck BMD and microarchitecture. Past PA was positively associated with tibial microarchitecture.”
In other words, current thinking is that physical activity you do today (or recently) can positively influence the BMD in your femoral neck area. Whereas, the BMD in the tibial microarchitecture (located near the ankle and a reasonable proxy for trabecular bone in the spine) is mostly influenced by physical activity you did in your early years (including your youth).
Study Details
Fifty community dwelling postmenopausal women were recruited for the study and subjected to physical activity. Bone structure was assessed by lumbar spine and hip dual-energy X-ray absorptiometry (DEXA), 3D modelling algorithms (3D-SHAPER) of hip DXA scans, and distal tibial high-resolution peripheral quantitative computed tomography (HR-pQCT) scans. We will define HR-pQCT in the next section of this post.
After examining the data, Dr. NG concluded that “past physical activity [had] lasting benefits for trabecular microarchitecture, and current physical activity [was] positively associated with cortical bone.”
If you are young, you can influence the bone structure of your spine (specifically the trabecular bone) through physical activity. Fortunately, you can influence the cortical bone in your femoral neck area with physical activity today.
Bone Quality vs Bone Density Measurements
The follow sections describes the various ways we measure bone density and bone quality. We will start with measuring bone density.
Bone Mineral Density (BMD)
Bone mineral density (BMD) tests are today’s most recognized tests to diagnose osteopenia and osteoporosis. However, as the name implies, BMD tests only measure bone density, not bone quality.
A second issue with BMD tests is the variability within the machines and even the same manufacturer over time. Several factors can influence your BMD test and t-score. A 2022 study from Sweden looked at this problem and identified several factors explaining the variability in the BMD and T-scores. (8)
Lack of information on bone quality is a problem. More than half of individuals who have low trauma fractures have BMD scores that are in the range of osteopenia.
Until recently, the average individual did not have access to bone quality testing. A high-resolution quantitative computed tomography test was the most common way of obtaining information on bone quality.
High-resolution peripheral Quantitative Computed Tomography (HR-pQCT)
High-resolution peripheral quantitative computed tomography (HR-pQCT), as the name implies, generates a high-resolution, three-dimensional monitoring of the architectural structure of bone. The word peripheral stands for our limbs as opposed to our torso. This microscopic view makes it good at determining the quality of bone in your forearms and lower legs.
HR-pQCT imaging is not practical for frequent use because it exposes people to higher amounts of radiation and costs more to operate. For these reasons, these tests are usually used for research or study in large hospitals.
Bone quality information is a key part of the decision-making process when someone is diagnosed with osteoporosis or osteopenia. The World Health Organization recognized the need for access to this information and created the Fracture Risk Assessment Tool, known as FRAX.
Fracture Risk Assessment (FRAX)
Some centers that provide DEXA testing will include FRAX scores with your BMD results. Your FRAX score is based on age, sex, weight, height, and other specific risk-related questions to determine your 10-year probability of a major osteoporotic fracture and a hip fracture.
To complete the FRAX questionnaire, you need the DEXA BMD result for your femoral neck. The FRAX does not take into account the BMD of your spine. If you have not received a FRAX score, you can follow MelioGuide’s tutorial to complete your FRAX.
If your spine score is lower than your femoral neck, you may be at a higher risk for fracture than predicted by FRAX.
Not all countries or clinicians use FRAX, but it should be considered one of many tools available to predict your fracture risk. A bone quality test on the market for the past nine years is the Trabecular Bone Score, or TBS.
Trabecular Bone Score (TBS)
What is a TBS test? TBS is a noninvasive, computer-generated calculation obtained via a software package that analyses the DXA scan. Having a test done feels and looks the same as having a DXA test.
The TBS indirectly estimates the microarchitecture of the trabeculae in the vertebral bodies of your lumbar spine and provides you with a score similar to the DXA BMD score.
Trabecular Bone Score testing has evolved to be important in assisting clinicians in making the right treatment decisions for their patients and monitoring the effectiveness of treatment on the quality of their patients’ bones.
In 2023, a panel of international experts concluded that TBS was a helpful tool for managing high fracture-risk women, men, and those with osteoporosis caused by secondary causes. (9)
There are a growing number of facilities around the world that provide this service. Unfortunately, access to TBS measurements is still relatively limited and expensive.
The newest test to enter the market originated in Italy and is called the Radio-frequency Echo-graphic Multi Spectrometry, or REMS for short.
Radio-frequency Echo-graphic Multi Spectrometry (REMS)
Radio-frequency Echo-graphic Multi Spectrometry (REMS) is a non-ionizing technology that uses ultrasound to assess the bone density and fracture risk of the neck of the femur and lumbar spine.
Unlike DEXA, it has been pre-programmed to recognize and exclude things that can skew the results, such as aortic calcifications, bone spurs, and other common artifacts that falsely raise DEXA scores.
Studies have shown REMS to be diagnostically accurate in comparison to DEXA. (10)
The REMS is not a bone quality test. It is, however, considered in certain populations to provide a more accurate bone density test. Nick Birch, cofounder of Osteoscan UK, told me that individuals with very arthritic spines or degenerative scoliosis can obtain more accurate readings with REMS than DEXA.
There is one thing that bothers me about the REMS test. The image of the spine in the report is a generic representation of a healthy spine.
No one has ever mentioned to my clients that the image on the report does not represent their spine.
Clients with known thoracic compression fractures have felt emboldened to take risks based on the REMS results of their lumbar spine. Please be cautious.
What is Bone Fragility?
A DEXA can indicate that you have a good bone mineral density score. However, your risk of a fragility fracture might be elevated, largely due to your reduced bone quality.
Conditions such as diabetes, chronic kidney disease, amenorrhea, and eating disorders can deteriorate bone quality.
Some clinicians use the FRAX in concert with the DEXA results to estimate fracture risk.
In the video interview above, I asked Dr. Rubin to describe bone fragility.
Factors That Affect Bone Quality
In this section, we cover the numerous health conditions and pharmaceuticals that can negatively impact your bone quality.
Co-morbidities, Pharmaceuticals and Bone Health
The following medical conditions can affect the quality of your bones:
- Diabetes (Type 1 or type 2)
- Hormone deficiencies (estrogen, testosterone, thyroid, parathyroid)
- High doses of thyroid medication
- Malnutrition or malabsorption diseases
- Cancer and cancer treatments
- Organ transplants
In addition, there are over fifty secondary causes of osteoporosis and over twenty pharmaceuticals that can negatively impact your bones. Speak to your doctor/pharmacist about possible alternatives if you are currently taking a pharmaceutical that has been linked to a lower BMD.
Genetics and Bone Health
We cannot control everything in life. We don’t get to choose our parents, however, genetics play a big role in the quality of our bones.
If you have a parent who has sustained a hip fracture (or if you have had a low trauma fracture on one of your vertebras or the long bones of your arms or legs while under the age of 45), you will likely be more susceptible to future fractures.
How to Improve Bone Quality
In this section, I identify steps you can take to improve bone structure and the quality of your bones. Let’s start with exercise.
Resistance Exercise and Bone Health
In their 2018 publication, Effects of Resistance Exercise on Bone Health (10), Hong and Kim state that “resistance exercise (RE) is known to be highly beneficial for the preservation of bone and muscle mass.”
They define resistance exercise (RE) as “a physical conditioning program that enhances fitness, health, and sports performance, using a variety of training modalities such as free weights, weight machines, medicine balls, elastic bands, and different movement velocities.”
Hong and Kim conclude that “based on the available information, RE, either alone or in combination with other interventions, may be the most optimal strategy to improve the muscle and bone mass in postmenopausal women, middle-aged men, or even the older population.
In particular, resistance exercise seems to be beneficial for the cortical bone.”
Studies dating back to 1984 (11) show that the type of exercise is equally important to protect from fractures.
Lifestyle choices and Bone Health
Your lifestyle choices can affect your bone quality.
- If you currently smoke, do your best to stop smoking.
- Do not exceed 2 alcoholic drinks a day.
- Reduce your intake of processed foods such as pastries, pizza, french fries, snacks, and refined grains.
- Reduce your intake of protein from cheese and processed meat.
- Build your diet around vegetables, fruit, whole grains, and healthy protein choices.
- Maintain a healthy body weight to ensure you maintain regular menstrual cycles.
Nutrition and Bone Health
In the article, Nutrients and Dietary Patterns Related to Osteoporosis, the authors write that “overall, adherence to a healthy dietary pattern including fruit, vegetables, whole grains, poultry, fish, nuts and legumes, and low-fat dairy products and the avoidance of processed food products will be beneficial for bone health, decreasing the risks of osteoporosis and fractures.” (12)
The article is a must-read for those looking to optimize their diet for their bones. Here are a few highlights:
Magnesium
Magnesium is important for bone health. It is involved in osteoblast proliferation.
Magnesium deficiency is associated with reduced bone formation (12). It is necessary for the activation of vitamin D, and it affects bone quality through its influence on the hydroxyapatite crystal size and formation.
Protein
The European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) recommends a dietary protein intake of 1.0–1.2 g/kg body weight/day, with at least 20 to 25 g of high-quality protein at each main meal.” (12)
The authors go on to say that “adequate protein intake is imperative for bone matrix formation and maintenance.” (12)
Consumption of adequate protein when strength training has been shown to improve the accretion of protein.
Ensuring adequate protein intake while strength training is an “important contributor to the maintenance of bone strength.
Other Nutrients and Foods
A bone-healthy diet includes a number of other nutrients and foods, including Vitamin K2, calcium, prunes, among others. A healthy gut microbiome that improves the absorption of nutrients can play an important role in bone health.
Conclusions
High resolution computer imaging technology has helped researchers learn more about bone strength, the importance of bone quality, and the limitations of solely relying on bone density to determine bone strength.
From these developments, we can conclude the following:
Bone Quality vs Bone Density
First, remember that your DEXA score is one variable in the overall equation for determining your bone strength. But it is not the be-all and end-all.
If you get a bone density score that is less than optimal, consider it an early warning signal indicating symptoms of osteoporosis. Unfortunately, for many people, the first sign of poor bone quality is a fracture.
Use the BMD score as an opportunity to take stock of all the variables that can affect your bone health.
Bone Quality, Bone Strength and Exercise
Second, the quality of your bone structure is very important in determining the strength of your bones and their ability to resist fracture.
It appears that people who are physically active have better quality bone structure. Create opportunities for safe movements and effective exercise that can influence the quality of your bones.
Balance Training
Third, your exercise plan should include balance training along with strength training.
Better balance leads to fall reduction. A lower fall risk leads to a reduced incidence of fracture.
Nutrition, Lifestyle Choices and Bone Quality
Fourth, make dietary and lifestyle choices that help your skeleton support you for your lifetime.
Low-Intensity Vibration Therapy
Lastly, if you are limited in your exercise regimen, consider low intensity vibration therapy as a surrogate for an exercise program.
Bottom line: bone quality matters. Eat well and incorporate physical activity into your bone health regimen. Consult with a qualified professional knowledgeable in movement and bone health to ensure safety and efficacy.
Further Readings on Prevention
References
- Beck TJ et al. Confounders in the Association between Exercise and Femur Bone in Postmenopausal Women. Med & Sc in Sports & 2011 Jan;43(1):80-9. doi: 10.1249/MSS.0b013e3181e57bab.
- McDonnell et al. Ann Biomed Eng 2007
- Delmas PD et al. J Bone Miner Res 2005
- Schuit SC et al Bone 2004
- Fonseca H, et al. Bone Quality: The Determinants of Bone Strength and Fragility. Sport Medicine. October 3, 2013
- Osterhoff G et al, Bone mechanical properties and changes with osteoporosis. Injury. 2016 Jun; 47(Suppl 2): S11–S20.
- Ng C-A, et al. Associations between physical activity and bone structure in older adults: does the use of self-reported versus objective assessments of physical activity influence the relationship? Osteoporosis International. 2020 Mar;31(3):493-503. doi: 10.1007/s00198-019-05208-y. Epub 2019 Nov 13.
- Karolina Lundstam, Kristin Godang, Mikkel Pretorius, Paul Markwardt, Mikael Hellström, Jens Bollerslev, Ansgar Heck, The Influence of DXA Hardware, Software, Reference Population and Software Analysis Settings on the Bone Mineral Density and T-Score Relationship, Journal of Clinical Densitometry, Volume 25, Issue 1, 2022
- Shevroja, E., Reginster, J-Y., Lamy, O., et al. (2023). Update on the clinical use of trabecular bone score (TBS) in the management of osteoporosis: results of an expert group meeting organized by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO), and the International Osteoporosis Foundation (IOF) under the auspices of WHO Collaborating Center for Epidemiology of Musculoskeletal Health and Aging. Osteoporos Int (2023). Published online: July 01, 2023: https://link.springer.com/article/10.1007/s00198-023-06817-4
- Adami G, Arioli G, Bianchi G, Brandi ML, Caffarelli C, Cianferotti L, Gatti D, Girasole G, Gonnelli S, Manfredini M, Muratore M, Quarta E, Quarta L. Radiofrequency echographic multi spectrometry for the prediction of incident fragility fractures: A 5-year follow-up study. Bone. 2020 May;134:115297. doi: 10.1016/j.bone.2020.115297. Epub 2020 Feb 21. PMID: 32092480.
- Sinaki M, et al. Postmenopausal spinal osteoporosis: flexion versus extension exercises. Arch Physical Med Rehabilitation. 1984 Oct;65(10):593-6.
- Muñoz-Garach A, García-Fontana B, Muñoz-Torres M. Nutrients and Dietary Patterns Related to Osteoporosis. Nutrients. 2020;12(7):1986. Published 2020 Jul 3. doi:10.3390/nu1207198





Comments
November 18, 2010 at 10:59pm
jean anne
Margaret ...... this was a useful read for me because I have a low reading in the lower back. It is good news to think that this does not necessarily mean "trouble" ahead ....... I will continue to exercise and eat with awareness. Also, I have trust and faith that all will be well for me as there is no family history of osteoporosis, although I know too that is no guarantee for me.
November 19, 2010 at 2:25am
Richard Martin
Jean Anne - I am glad you found the article useful and keep up the exercise and good nutritional habits.
- Margaret
November 20, 2010 at 6:24pm
Marion Kregeloh
Only strong bones can resist fractures. It is official now, after all. Thank you, Margret, for a great program! DXA low or high, what matters is the HOW of exercise and nutrition.
November 22, 2010 at 2:17pm
Richard Martin
Hi Marion - Thanks for the comments. Yes, the HOW of exercise and nutrition does matter. Health professionals such as you who know these "hows" are what will make the difference for clients. Keep up the good work in California!
- Margaret
February 2, 2011 at 7:00pm
Ed
I found the article to be very encouraging! I am only 40 years old and have been diagnosed with severe Osteoporosis, having a bone density of -4.1.
The only reason I know about the condition is because I had a low vitamin D level of 20, so they did a DXA scan that revealed the problem.
My vitamin D levels are now high, and all of my other medical tests appear normal.
No one knows the cause of my Osteoporosis, but it's probably many things. Low vit D, small frame, too sedentary, anxiety, caffeine,etc.
I've been terrified about getting a fracture.. but hopefully will be able to reverse and improve my condition.
I don't believe I'll ever be willing to take any of the medications they recommend.
Perhaps some doctor will give me the HR-pQCT, but I'm concerned about radiation, having done alot of x-rays and a CT in the past year or so.
Thank you Margaret.
February 4, 2011 at 8:27am
Richard Martin replies
Ed - Thanks for the update and keep us posted on your progress. Glad that the article was of use to you. There is still much research to happen in this area. As it happens, I will keep you posted. Keep in mind that exercise for osteoporosis should be a part of your health routine.
A couple of things - in case it has not been done - is to ask your doctor to check your testosterone level and for celiac or gluten intolerance (many people do not realize they are celiac). It is good that your doctor had your Vit. D level tested and then followed up with a DXA. Sounds like your in good hands.
February 19, 2011 at 2:12pm
Theresa Hunter
This article was very interesting and would seem to account for why some people with low bone density/osteoporosis don't fracture and others do.
The rheumatologist I'm currently seeing does place emphsis on exercise, which is good, but he also feels that those with osteoporosis (like myself) who are classified as having "low" fracture risk do not need to make any changes to their daily activities, body movements or exercise routines. This doesn't make sense to me, which is why I sought out more information on line and, happily, found your site. I think part of his reasoning is based on my age (48). Given that a DXA scan doesn't reveal all we need to know about our bones, shouldn't everyone with osteoporosis, at low or high fracture risk, be taught to actively avoid potential fractures through exercise and postural/body movement changes? He thinks that flexion exercises and stretches don't put me at fracture risk because I'm considered at "low" fracture risk. What do you think based on research and experience?
Thank you for all the great information.
February 19, 2011 at 7:45pm
Richard Martin replies
Theresa, your comments and questions are great. I encourage you to follow your intuition.
As you have correctly stated bone mineral density scores are not the only determinant of fracture risk and so it is best to be preventative. There are also additional benefits to being mindful about how you do your exercises and daily activities. It reduces your risk for disc and muscular injuries. Secondly, as you incorporate safe mechanics into your exercise routines it reinforces good body mechanics through your daily activities, and so they support one another. Thirdly, 99.9% of people in society have more flexion (forward bending) of their spine than they need and do not need to add more into their exercise routine - quite the opposite. Lastly, your "fracture risk" may change in the coming years as you go into menopause and so it is never too early to start moving with stronger, safer body mechanics.
October 30, 2011 at 5:42am
jessica walker
As a physiotherapist I have found this online course fantastically informative so far. I have passed it on to my colleagues on facebook as I think its a message we should all be passing on to our patients. Thank you!
October 30, 2011 at 3:25pm
Margaret Martin replies
Hello Jessica,
Thank you for passing the information onto your colleagues. It helps spread the word on our important role into our patients skeletal health. Be well.
Margaret
December 10, 2012 at 3:28am
Sylvia Morgan
This article has made me feel much better, thank you. I have just had a regular scan which revealed osteoporosis in my spine. My GP wants me to start on Bonviva. Having researched this I am very reluctant. I have always been very active and physically fit so intend to rigorously follow the right exercise plan and beneficial diet for my bones for the foreseeable future.
May 7, 2018 at 11:12pm
Betty
I am 58 year old female who has exercised my whole life and have suffered 2 vertebral compression fractures in the last two and a half years, one traumatic and one not. I have significant osteoporosis in my spine with a T score of -5 which has improved on one year of Forteo. I used to run 3 miles a day up until my first fracture. Is it safe til still at least jog because I am afraid to do a lot of things I used too!
May 8, 2018 at 8:15pm
Margaret Martin replies
Hi Betty, You can certainly be doing intelligent, safe strength training, balance exercises and brisk walking. You should stay within the Beginner and Active Level strength exercises in my book Exercise for Better Bones. Your Forteo treatment is coming to an end, they usually recommend 18 months. Once your bone density is redone your question is a valid one to discuss with your doctor. I cannot give you a definitive answer because I do not know what your posture looks like, your running style or your current bone status. All the best, Margaret
March 2, 2019 at 6:39pm
Betty L Abolafia-Rosenzweig
Can you site the reference for where you mentioned" Another study suggests that people who are more active through exercise have better bone quality than people who are inactive: " I would like to read it . Thank you!
March 6, 2019 at 7:25am
Richard Martin replies
Hi Betty: http://melioguide.com/osteoporosis-prevention/bone-quality-osteoporosis/ Read under the title Bone Quality Matters.
All the best,
Margaret
May 9, 2021 at 4:46am
Moon
I’m in my mid-50s and was recently diagnosed with severe osteoporosis of the spine (-4.4) — grateful to have found your site with such comprehensive and insightful information. Does loss of height indicate compression fracture or is it in any way related to bone quality? Also, is there any relationship between osteoporosis and arthritis of the spine (L1-L4)?
Many thanks,
May 11, 2021 at 1:13pm
Chris
Hi Margaret. I have just completed active level of your Exercise fir Better Bones. Loving this! I am feeling stronger by far. I do have osteoporosis-2.5 and due for dexa scan June 1. I have decided not to take any biphosphonates at this time and instead will continue exercising as well as taking collagen and calcium. Your thoughts on bypassing Reclast and/or Prolia would be appreciated as this was a difficult decision. I have lost height ( one and a half inches) and an 69 years old. Osteoporosis is in family history and I worry about shrinking! Thank you again for your wonderful book and videos which demonstrate exercises. So very helpful!!
May 11, 2021 at 2:23pm
Richard Martin replies
Hi Chris. Thank you for your update and congratulations on your commitment to your exercise program. Margaret is unable to comment on any individual case in the absence of a consultation. Every person is unique in their own way and she needs to look at that individual before providing advice. You can check out her service here: https://learn.melioguide.com/individual-coaching-60-minutes
May 11, 2021 at 6:37pm
Connie Pierson
Hi Margaret I purchased the $70 posture series online in the fall. I was unable to complete the series because of pain from compression fractures. I have been through X-ray and MRI tests and in physical therapy for six months. Can I still access the course? Thank you.
May 11, 2021 at 7:51pm
Richard Martin replies
Hi Connie. Yes. You still have access to the course. You can login here:https://learn.melioguide.com/30-day-posture
If you forget your password, please visit here: https://learn.melioguide.com/forgot-password
May 13, 2021 at 11:35pm
Laura M Theis
What can I do for building bone? My doc said discontinue calcium supplement due to kidney stones.will exercise and diet work in place of cal ium? Thanks Laura T