Table of Contents
If you have sleeping problems you should read The Sleep Solution — Why Your Sleep is Broken and How to Fix It by Dr. Chris Winter. Most nights my sleep is “fragmented” — meaning that for more nights than I like, I wake up and experience problems getting back to sleep. I suffer from sleep maintenance insomnia.
The Sleep Solution helped me understand why my sleeping pattern was broken and what I need to do to improve the quality my sleep. I describe my personal journey to fix my sleep using Dr. Winter’s book.
I also discuss the relationship between quality of sleep and bone health — something that should interest most readers. In December of 2021 I completed a sleep study to determine if there were issues that affected my sleep. I report on that experience in this post and provide recommendations (not provided by my health provider) that will make your sleep study more successful.
Later in this article, I cover two other important sleep training books, Why We Sleep by Dr. Matthew Walker and The Effortless Sleep Method by Sasha Stephens.
I also discuss a 2018 book on the importance of circadian rhythm, The Circadian Code, by Satchin Panda, PhD. One of the interesting findings in Dr. Panda’s book was how circadian rhythm affects bone health. I cover this later on the blog post and encourage readers to review this.
Sleep, Osteoporosis and Low Bone Density
This site is dedicated to bone health and osteoporosis prevention and management. As a result, before I get into the book reviews, I should discuss the relationship between osteoporosis and sleep. When it comes to keeping our bones strong, sleep plays a very important role in at least five ways.
High quality sleep:
- Improves the absorption of nutrients and reduces gastrointestinal problems.
- Changes our food choices. When we are sleep deprived, we crave high calorie foods.
- Enhances our gut bacterial community.
- Leads to better balance and reduces our injury and fall risk.
- Reduces cortisol production.
Each of these is covered in detail in Why We Sleep.
Shortened Sleep Associated with Low Bone Mineral Density and Osteoporosis
A study published in the Journal of Bone and Mineral Density in November of 2019 identified a link between short sleep and low bone mineral density and osteoporosis (1). The research team examined “a sample of 11,084 postmenopausal women from the Women’s Health Initiative. They performed a cross-sectional study of the association of self-reported usual hours of sleep and sleep quality (WHI Insomnia Rating Score) with whole body, total hip, femoral neck, and spine BMD using linear regression models.” (1)
The study stated that women reporting 5 hours or less per night had:
- 22% and 63% higher risks of experiencing low bone mass and osteoporosis of the hip, respectively. Similar results were seen with the spine.
- Lower BMD at all four sites assessed—whole body, total hip, neck, and spine—compared with women who reported sleeping 7 hours per night.
The main author, Heather Ochs-Balcom, PhD of the University of Buffalo, stated: “Our study suggests that sleep may negatively impact bone health, adding to the list of the negative health impacts of poor sleep. I hope that it can also serve as a reminder to strive for the recommended 7 or more hours of sleep per night for our physical and mental health.”
Later in this article, the section on The Circadian Code, I discuss the relationship between the circadian rhythm.
Clearly, sleep plays a critical role in our health. We are now starting to see that there is a relationship between sleep and osteoporosis.
The Sleep Solution by Chris Winter
The Sleep Solution is much needed, especially for those of us in search of better sleep. I have read many blog articles on sleep and, for the most part, I find them repetitive and uninformative. They tell you that your health is at risk if you do not sleep, that you need a certain number of hours of sleep per night, and finally that you should sleep in a dark, cool room and not take your computer or iPhone to bed with you.
The problem is that the people who read these articles usually have sleep problems, often follow all of these guidelines and still cannot sleep. The reader is left with a sense of failure and anxiety — which furthers the sleeping problem!
The Sleep Solution Approach
Dr. Winter does not take this approach. He insists that you read the book from beginning to end so that you learn the basics of sleep and understand what is happening to your sleep. Instead of simple and obvious rules, he challenges the reader with two facts.
First, many of us dysfunctional sleepers insist that they do not sleep and have not slept for years. How can that be true? If, every night, you did not sleep, you would likely be dead — but you are here, reading this article I have written, and very much alive.
Second, we have an emotional relationship with our sleep. Most of the problems we have with sleep stems from the dysfunctional relationship we have with our sleep. (Sleep problems cause by physical issues such as apnea are different from emotional issues and demand specific treatment protocols). As a result, Dr. Winter encourages the reader to come to terms with this relationship and, like any relationship having a rough patch, put some effort into making it work.
The Sleep Solution: Reference Guide for Sleep Disorders
Dr. Winter has treated thousands of patients for various sleep disorders. He spends a significant amount of his time educating patients on the basics of sleep and this book was written as a reference guide for his patients.
We are fortunate that he published The Sleep Solution and made it available to you and I, the general public. For a modest price, you can access much of the information he shares with individual patients.
The Sleep Solution Deliverables
In The Sleep Solution, Dr. Winter achieves the following:
- Delivers a comprehensive explanation of how sleep works. He covers the stages of sleep and why they matter, how circadian rhythms work, and the chemical foundations of wakefulness and sleepiness and how the two states compete with each other to keep you awake or put you to sleep.
- Addresses many of the myths and misunderstanding about sleep that confuse many of us with sleep problems and the physicians who treat people with sleep problems.
- Clarifies the difference between sleep deprivation and insomnia. This is one of the most important parts of the book. Instead of attempting to explain the difference in this blog post, I will leave it to you, the reader, to read his book to learn about this topic. Dr. Winters does a far better job than I ever will explaining this complex issue.
- Asks the difficult questions about their sleep and challenges many of their beliefs. I feel that this discussion is one of the most important contributions of this book. The better understanding you have of your sleep behaviour, the greater the chance that you will fix your sleep problems.
- Presents the latest research available on sleep and, where pieces are missing, he fills in with his own informed opinions.
A Sense of Humour
One more thing before I cover the book in more detail: Dr. Winter presents the material in a friendly and accessible manner. He is self deprecating and has a goofy sense of humour. Here is a gem from the chapter on snoring and apnea:
“When I turned thirty, I remember Ames (Dr. Winter’s wife) telling me that if I rolled over on my back, I sawed some logs. For years, like most men who come to my clinic, I assumed my wife was lying. Everyone knows that women have nothing better to do than to accompany their husbands to doctors’ appointments and make up stories about their spouses’ breathing at night.”
Introduction to Sleep Medicine
The Sleep Solution is broken into two major sections. The first section is an introduction to sleep medicine and the second section (after an “intermission”) addresses sleep problems and how to deal with them.
Dr. Winter provides a thorough explanation of sleep in the first section of the book. By now most of us know that sleep is important to our health and that poor sleep can detrimentally affect our heart, mood, immune system, and brain, can lead to weight gain, and has been linked to cancer. He covers each of these issues but, thankfully, he does not overdo the message.
On the other hand, he does point out several important new findings from recent research on sleep and the brain. For example, in 2015, University of Helsinki researchers Antoine Louveau and Aleksanteri Aspelund found that the brain has a system for removing waste called the glymphatic system (2). This system is 60% more productive when we sleep as compared to when we are awake. Removal of waste products in the brain plays an important role in long term cognitive well-being.
Sleep is Essential and Will Happen
Sleep is essential to our survival. Dr. Winter points out that our brain insists that we sleep. Eventually, no matter how poor the quality of your sleep or how sleep deprived you are, you will fall asleep. You might find the road to sleep to be a rocky one, but sleep is something that happens to all of us (even Rolling Stones guitarist Keith Richards).
Dr Winter points out that most people he sees do not grasp this simple concept. Many insist that they “haven’t slept in years.”
Really? You might have restless nights, you might not like the quality of your sleep, but you do sleep.
Some individuals, on the other hand, are sleep deprived. People who work night shifts are often sleep deprived. There are sleep tests that allow you to determine if you are sleep deprived and Dr. Winter provides several in the book. I completed each of these self-assessments and learned that I do, in fact, sleep at night. I just needed to work on improving the quality of my sleep.
Sleep Deprivation, Fatigue and Poor Sleep
This book made me think about the difference between sleep deprivation, fatigue, and poor sleep. Understanding these differences is essential to the sleep remedies described later in the book.
The chapter entitled Sleep Stages delivers an excellent overview of the structure of sleep and why it is important that your transition between the different sleep stages in the correct order. I appreciated the explanation of the different sleep stages when, later in the book, Dr. Winter discusses sleep studies.
During a sleep study, the sleep technician generates a reading of your sleep pattern called a polysomnogram. I was able to leverage my learning from the Sleep Stages chapter to interpret the output from a polysomnogram.
How to Treat Sleep Problems
Once you have a firm understanding of your sleep, Dr Winter moves onto how to treat sleep problems. This is the second section of the book. Like many sleep specialists, he discusses the importance of sleep hygiene. He also covers treating insomnia, sleep schedules, napping, snoring, apnea, sleep medications, sleep studies, sleep efficiency, sleeping aids and other sleep conditions.
I have read several books on sleeping, including Say Goodnight to Insomnia by Dr. Gregg Jacobs, and feel that The Sleep Solution is the most comprehensive, practical, pragmatic and realistic of them all.
Two other books require mention.
- Why We Sleep by Dr. Matthew Walker is the latest addition to the sleep reading list.
- The Effortless Sleep Method published in 2010 by Sasha Stephens is another important contribution to this field.
I discuss both books, in detail, later in this blog post.
Trazadone
As well as tips, self assessments and directions, it includes a number of surprises. For example, I was alarmed to learn in the chapter on sleep medications that the most common sleep medication prescribed by physicians is not even a sleep medication! It is an FDA approved anti-depressant: Trazadone. This is concerning.
As Dr. Winter points out in The Sleep Solution: “There is no real literature supporting their [anti-depressants] off-label use in helping patients fall asleep faster or even stay asleep. To me, these drugs epitomize the haphazard, misinformed, and dangerous practices of some doctors who do not understand sleep or how to treat it.”
Did The Sleep Solution Solve My Sleep Problems?
Several months have passed since I first wrote and published this review in July of 2018. The section you are now reading was added in September 2018 to update you on my personal journey with The Sleep Solution.
Since publishing the review in July, a number of people have asked me if reading the book and employing the techniques provided by Dr. Winter improved my sleep. In other words, was The Sleep Solution the solution to my sleep problems?
The answer is yes. The Sleep Solution worked because it did two things for me.
The Sleep Solution Helped Me Understand Sleep
First, the book gave me a better understanding of sleep. I learned that I sleep during the night. Unfortunately for me (and most problem sleepers), my sleep patterns are dysfunctional and my sleep quality is poor. Just knowing I do sleep at night (although it does not feel like I do) reduced my ongoing anxiety about my sleep.
Sleep Restriction Therapy (The Ice Bucket Sleep Challenge)
Second, I learned that dysfunctional sleep can be fixed through Cognitive Behavioural Therapy (CBT). Dr. Winter discourages the use of pharmaceuticals and advocates CBT as the path to good sleep. There is an abundance of clinical research supporting the effectiveness of CBT and, as a further bonus, CBT means you do not need to take medications or supplements to fix your problematic sleep.
Dr. Winter recommends a protocol that is part of CBT he amusingly calls the “Ice Bucket Sleep Challenge”. No need to worry. No-one will be dumping ice water on you. The clinical name for it is sleep restriction therapy (SRT). It is very effective but, I should warn you, it is not fun and requires serious commitment.
The objective is to increase your sleep efficiency. I was spending too much time in bed and not enough of that time was spent sleeping. In other words, my sleep was inefficient.
How Sleep Restriction Therapy Worked For Me
Here is how sleep restriction therapy worked for me. I restricted the duration of my time in bed to five hours and thirty minutes a night. I would go to bed a 12:30 AM and get up, whether I liked it or not (and most time I did not like it), at 6:00 AM. Although I felt groggy each day and wanted to nap, I didn’t. This protocol trains the brain’s clocking system, the suprachiasmatic nucleus, that a new sleeping pattern is in town.
I followed this protocol every night — without exception. It took a week to 10 days until my brain and body capitulated and I eventually slept through my first full night of uninterrupted sleep in years. It took another 20 to 25 days before I settled into a regular healthy sleeping pattern. In total, it took over a month to regain control of my sleep.
Those first 10 days were complete misery. When I take a dislike to people, I recommend they try this exercise. (Just kidding.)
Once I felt confident that my brain was retrained and healthy sleep was established, I added 15 to 30 minutes to my nightly sleep.
How to Succeed With Sleep Restriction Therapy
I found it very difficult staying awake each night until 12:30 AM. I like to read at night but found with this protocol I was unable to read because I fell asleep before my prescribed sleeping time. To stay awake, I went out late each evening for long, long walks. I not only fixed my sleeping problem, I added some extra exercise to my day. Pretty good deal!
I recommend you do this protocol during the spring, summer or fall seasons when walking at night is accessible and pleasant. Also, I found it relatively easy to stay awake through the long and sunny days of July and August.
Following this protocol during January and February in northern climates when the days are short and the light is low could be a challenge, unless you have access to a treadmill or exercise bike at home. If you are one of the lucky ones who gets away from the winter weather, perhaps now is your opportunity to fix your broken sleep while enjoying the nice weather!
One more point regarding time of year. I think it’s best to do sleep restriction therapy when the days are long and warm and the evenings are cool. Cooler temperatures at night are more conducive to good sleep.
If you experience dysfunctional sleep and you know that the cause is not a physical impairment such as apnea, I encourage you to try this approach. I think that you’ll find that, as the French say, ca vaut la peine.
Where to Purchase The Sleep Solution
You can purchase The Sleep Solution on Amazon in paperback. Please note I receive small commission from Amazon if you purchase the book.
About Dr. Chris Winter
Dr. Winter is a physician, a board certified sleep-medicine specialist, and a board-certified neurologist. He has been involved in sleep medicine and sleep research since 1993 and is the owner of Charlottesville Neurology and Sleep Medicine clinic in Charlottesville, Virginia where he has been practising sleep medicine since 2004.
Conclusion to The Sleep Solution
Dr. Winter has done the poor sleepers of the world a great service with the publication of the book, The Sleep Solution. I encourage you to read it so that you can learn more about your sleep and how to make it better.
The Sleep Solution is now available on Amazon in paperback.
Exercise Recommendations for Osteoporosis
Exercise is an essential ingredient to bone health. If you have osteoporosis, therapeutic exercise needs to be part of your osteoporosis treatment program.
But what exercises should you do and which ones should you avoid? What exercises build bone and which ones reduce your chance of a fracture? Is Yoga good for your bones? Who should you trust when it comes to exercises for osteoporosis?
A great resource on exercise and osteoporosis is my free, seven day email course called Exercise Recommendations for Osteoporosis. After you provide your email address, you will receive seven consecutive online educational videos on bone health — one lesson each day. You can look at the videos at anytime and as often as you like.

I cover important topics related to osteoporosis exercise including:
- Can exercise reverse osteoporosis?
- Stop the stoop — how to avoid kyphosis and rounded shoulders.
- Key components of an osteoporosis exercise program.
- Key principles of bone building.
- Exercises you should avoid if you have osteoporosis.
- Yoga and osteoporosis — should you practice yoga if you have osteoporosis?
- Core strength and osteoporosis — why is core strength important if you have osteoporosis?
Enter your email address and I will start you on this free course. I do not SPAM or share your email address (or any information) with third parties. You can unsubscribe from my mail list at any time.
Richard’s Overnight Sleep Study (Polysomnogram)
In late 2021 I asked my physician if I could have an overnight sleep study (known as a polysomnogram). My sleep has improved since using Dr. Winter’s protocols but it was still fragmented.
I wondered if there were other issues at play — physical impairments such as sleep apnea — that were affecting my sleep quality.
My physician was able to arrange an overnight sleep study at a hospital near my home. The following is a summary of my experience and the outcome, as well as tips and suggestions that could make your sleep study experience a success.
The Sleep Study Process
Once the sleep study was scheduled, I received instructions from the sleep lab at my local hospital on how to prepare for the event.
They recommended that I:
- Avoid sleeping (napping) during the day of the study.
- Not consume medications or alcohol before the sleep study and to take any medications to the session for the technician to review.
- Limit (or eliminate) caffeine during the day of the study.
- Bring comfortable pyjamas.
- Optionally, bring my own pillow.
My session was scheduled to start at 10:00 PM and the staff member told me to be at the hospital at 9:30 PM for registration. I arrived, registered and within 10 minutes a sleep technician welcomed and invited me into the secure sleep lab area. The technician showed me where the bathroom was and escorted me to the room I would sleep in that night.
She showed me room layout and identified the call button I could use to request her attention. I was told that the session would start when I was ready to go to sleep and that it would end at 5:45 AM the next morning. If I was still asleep at that time, they would wake me at 5:45 AM and ask me to leave.
At this point, she asked me a series of questions:
- Do I snore?
- Am I on medication?
- Do I have restless legs when I slept?
- What was my typical night of sleep?
Once that was out of the way, she said she would leave the room and asked me to put on my pyjamas while she was away. After I got into my pyjamas, I used the call button next to the bed to have her return.
Polysomnogram Set Up
When she returned she wired me for the pleasant night of sleep ahead. The configuration included the following items:
- Chest strap that measured my breathing pattern.
- Series of electrodes taped to my scalp to measure electrical activity on my brain.
- More electrodes [electro-oculogram (EOG)] positioned near my eyes to measure eye movements.
- Electrocardiogram connectors attached to my chest to measure heart rhythm.
- Nose cannula to monitor air flow.
- Microphone attached to my chest to monitor snoring.
- Electromyography connectors attached to my shins to monitor muscle activity.
- A peripheral capillary oxygen saturation monitor (clipped to my index finger) to measure continuous oxygen saturation.
All of the cables (from all of the attachments) terminated into a small red box. The small red box, in turn, had cables leaving it that terminated into a large wall panel. The data would be sent during the night to the technician for monitoring.
The image above is a selfie of me in the bed with the connectors and cables. You can see the small red box in the top right hand corner of the image. The cables attached to my body terminated in the box. The box had a cable that connected into the wall panel.

How Much Sleep Data Do They Need?
As she attached all of the connectors I asked my technician how much continuous sleep I needed to provide so that she could give my physician a usable sleep report. She told me she needed two continuous hours of sleep.
I was concerned because I usually do not sleep well in a new setting, and this setting was particularly uncomfortable. I anticipated that I might “fail” the test and not deliver the required amount of sleep data.
She told me that quite a few people are unable to provide adequate sleep data and, in some cases, people are so uncomfortable that they leave the premises shortly after putting their head on the pillow.
When everything was set up, the technician left the room and went to her lab position. She spoke over the speaker into my room and asked if we could do a series of tests. She asked that move my eyes in different positions to calibrate the electro-oculogram (EOG) attached near my eyes. I was also asked to vary my breathing pattern.
The Sleep Study Experience
When the sleep technician finished the configuration and test process, I was ready to settle down into sleep.
I brought a book to read and lasted about ten minutes; at which point I asked the technician to shut off the lights. What followed was one of the worst sleeps I have ever experienced.
It struck me as ironic that you go to a sleep lab to study your sleep (because you are a bad sleeper), only to find that you are trying to sleep in the most uncomfortable setting possible. If you are a bad sleeper (at the best of times), expect to have an even badder sleep at a sleep lab.
This is an important fact bad sleepers should know before they go to a sleep bad. Make sure you do everything you can beforehand to cause you to fall and stay asleep. More on this later.
A Challenging Night
These are the things that challenged my sleep that night:
- The cables attached to my head, chest, shins and the tip of my finger were very uncomfortable. I could move around, and shift to sleep on my side, but I have to move the cables and reposition them with each change. Not fun.
- I do not sleep well in new locations and while the hospital tries its best, the room is very sterile and, well, like a hospital bed.
- Hospital sounds. Several times during the night, a voice came over the PA system with an announcement. “Code Blue on Floor 3. Code Blue on Floor 3.” I didn’t know what a Code Blue was and I hoped I was not the cause.
- At one point during the night, I had to go to the bathroom. I called the technician. She disconnected the small red box (that terminated all of the connectors) from the wall panel, strapped the box over my shoulder and told me I was free to go to the bathroom. When I returned she reconnected the small box to the wall panel.
- My sleep continued to be disjointed and eventually at 5:00 AM, I threw in the towel. I tried my best but was unsure whether I generated two hours worth of sleep data. The technician came in, quickly detached all the connectors, whereupon I dressed gathered my things and headed home.
How to Prepare for a Sleep Study
If you are challenged to have a good night’s sleep at home, you will find the experience at a sleep lab to be difficult. You do not want to have to go back and have another test.
To improve your chances of providing two continuous hours of sleep data, I recommend the following:
- The most important thing you can do is to reduce the amount of sleep the night before the event. The stronger the urge to sleep (because you are sleep deprived), the better the chance you will give them their two hours of sleep data. I cannot emphasize this enough.
- Have a coffee-free the day of the sleep test.
- You probably will not know the temperature of the room until you get there. I suggest you bring two pairs of pyjamas, a light pair for warmer ambient temperatures and a heavy pair for cooler sleeping conditions.
- Bring warm socks. Just in case.
- Your pillow will make the environment more familiar. I suggest you bring your own.
Results From My Sleep Study
Two weeks after my sleep test, my physician called to tell me that they managed to get the data they needed to assess my sleep.
The good news was that my sleep is normal.
The bad news is that my sleep is normal and I know less about why my sleep is fragmented.
I realized that I am as not a disciplined with my sleep as I need to be.
Sleep comes naturally to some people. I am not one of those people and so I need to be a bit more attentive to how much I sleep, when I go to bed, and when I get up.
The Winter protocol showed me that I only need seven hours of sleep. I need to be respectful of that and limit my sleep to what I need so that I reduce the fragmentation of sleep.
Why We Sleep by Matthew Walker
Matthew Walker is a leading expert on sleep. He is a professor of neuroscience and psychology at University of California (Berkeley) and director of its Sleep and Neuroimaging Lab. His book, Why We Sleep, provides new insights (based on the latest scientific research) into the role of sleep, how we have disrupted our sleep, and what we can do (at both the individual and societal level) to get it back to its natural order.
In his book, Dr. walker states that the latest research into sleep has “an unequivocal message: sleep is the single most effective thing we can do to reset our brain and body each day — Mother Nature’s best effort yet at contra-death.” His concern is that this message has not gotten to the public and his book “is intended to serve as a scientifically accurate intervention addressing this unmet need.”
Much of the book covers why sleep matters to our health and well being. This may not be of interest to people who already know that they have poor sleeping patterns and may add to their existing anxiety. However, the book does provide insights into what could be wrong with your sleep and what you should do to fix it. Because it is based on the latest research presented by an expert in the field of sleep and since education is a key component of CBT-I, I recommend that people who want to improve their sleep read Dr. Walker’s book.
In the book’s opening chapter, Walker states that you do not have to read the book in its entirety and should freely read chapters that interest you. I found this to be liberating since his approach to each topic is very accessible.
Why Our Sleep is Dysfunctional
Walker explains that the easy availability of incandescent light, blue light, caffeine, and alcohol and rigid work (and school) schedules has disrupted the gift of sleep — a natural therapeutic that took Mother Nature millions of years to perfect. All of this happened in the last 100 years — the blink of an eye in evolutionary terms. Walker points out that daily sleep duration in the developed, western world has decreased by about 25% since 1930 — from about 8 hours a day to 6.5 hours.
Sleep, The Circadian Rhythm and Adenosine
Walker does a wonderful job describing the relationship between our circadian rhythm (our internal clock that orchestrates many of our biological activities, including wakefulness) and adenosine levels in the brain (the chemical that creates sleepiness). These two systems are independent and play a critical role in when we sleep. When the relationship between the two systems gets out-of-whack, the outcome is a dysfunctional sleep pattern.
For more on circadian rhythm, I encourage you to read the review of The Circadian Code later in this article.
Are You Getting Enough Sleep?
There are more than a hundred undiagnosed sleep disorders. The most common is insomnia. This is followed by sleep disordered breathing (sleep apnea).
Dr. Walker states that a clinical sleep assessment is the correct way to determine if you are getting enough sleep, the probate cause and best solution. He recommends that if you suspect that you or a loved one has a sleep disorder, that you consult your physician and request a sleep assessment.
However, in the absence of this tool, he does provide some rough guidelines that can help you answer this question. If either of the following are true, you are likely not getting adequate sleep:
- You could easily fall asleep at ten or eleven a.m. after a night of sleep.
- You need coffee before noon to function optimally.
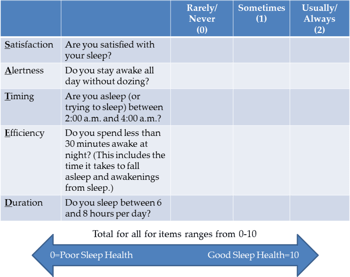
In addition, Dr. Walker provides another resource, a questionnaire called SATED developed by the American Academy of Sleep Medicine (AASM), that you can use to evaluate your sleep. I have included it here.
Insomnia
Dr. Walker devotes a chapter to sleep disorders. I will not cover all of these in this post. Instead, I’ll quickly cover the key points on insomnia.
As I mentioned earlier, insomnia is the most common sleep disorder. There are two types of insomnia. Onset insomnia refers to difficulty falling asleep. Maintenance insomnia refers to difficulty staying asleep. Some unfortunate individuals suffer both conditions. Dr. Walker notes the diagnosis of insomnia as:
- Dissatisfaction with either quantity or quality of sleep.
- Daytime impairment.
- Three nights each week of insomnia for a period of three months.
- Absence of co-existing mental disorders or medical conditions that could be causing sleep disruption.
These are not meant to encourage self diagnosis but act as a signpost indicating insomnia. You should consult a sleep professional if you suspect you have insomnia.
Five Things That Could be Stopping You From Having a Good Night’s Sleep
A number of variable can affect (and disrupt) your sleep. Broadly, sleep hygiene and your attitude towards your sleep have considerable impact on the amount and quality of sleep. Sleep therapy is designed to address these two forces. Besides these two categories, Dr. Walker discusses five things he believes have a detrimental affect on sleep.
Caffeine
Dr. Walker devotes a lot of time to how caffeine disrupts our sleep. He describes how the daily buildup of a chemical in the brain, adenosine, creates “sleep pressure” – the desire to sleep. Caffeine mutes adenosine and makes us feel more awake and alert. It competes with adenosine for access to receptors in the brain that trigger sleepiness. While it occupies the receptors, the desire to sleep diminishes.
Caffeine has a half life of five to seven hours. Half life refers to the time it takes the body to remove 50% of a chemical’s concentration. Dr. Walker uses the following example to illustrate caffeine at work. Say you have a cup of coffee at 7:30 pm — after evening dinner. Fifty percent of that caffeine dose is still in your brain and blocking sleep receptors at 1:30 am. That concentration can be enough to disrupt your sleep. Further, it takes another 7 hours to remove 50% of that 50% concentration. In other words, you will wake up with 25% of the caffeine you consumed after dinner last evening still in your system and actively suppressing adenosine.
Some people are more effective at “burning off” the caffeine dose than others. You might or might not be one of those. Regardless, if you have sleeping problems and you are a consumer of caffeine, you should consider only drinking a small amount first thing in the morning or eliminate it altogether.
Caffeine Little Known Facts
Dr. Walker encourages the reader to keep in mind a few more important items related to caffeine.
- There are many sources of caffeine including coffee, colas, tea, and some medications.
- De-caffeinated does not mean non-caffeinated. It means a reduction in caffeine concentration.
- When the caffeine finally wears off, the adenosine (that has been building up during the time the caffeine is active) can cause a “crash” or sudden urge to sleep. This crash could happen at inopportune times like during a meeting, which could be embarrassing, or while driving, which could be fatal.
How Much Caffeine Can You Drink?
If you are a coffee drinker and enjoy the caffeine experience you will probably not like what Dr. Walker says about the relationship between caffeine consumption and quality of deep sleep.
Dr. Walker acknowledges the existence of rapid metabolisers — individuals who are able to quickly process and break down caffeine because of an enzyme. You know someone like that! Rapid metabolisers are less sensitive to caffeine and can sleep after having coffee.
For many people, caffeine is “wake promoter” and can slow the arrival of sleep. For most people, Dr. Walker states that caffeine affects sleep quality — particularly deep sleep. So while you may be able to drink coffee and easily fall asleep, your deep sleep is compromised.
Dr. Walker points to two studies to make his point.
In the first, a standard 180 mg dose of caffeine is given to a group of research subjects in the evening. They fall asleep but the amount and electrical quality of deep sleep is compromised. A 20% reduction in deep sleep quality was experienced by the participants — equivalent to adding 25 years to your age!
In the second study out of Surrey UK, the research team gave participants a standard caffeine dose in the morning (7:20 AM, on average), provided no caffeine during day, and asked the participants to go to bed by 11:00 PM.
The researchers reported that even the early morning only caffeine dose disrupted deep sleep quality — to the effect of a 10 to 12% drop in deep sleep quality.
My Personal Caffeine Experience
Since learning Dr. Walker’s position on coffee consumption and sleep, I decided to eliminate coffee from my day. It was not easy. I love a cup of coffee!
Initially I reduced my coffee intake and limited it to a 7:00 AM dose. But within a few days of stopping completely I noticed that my sleep was much, much better. Maybe Dr. Walker is right, after all.
Modern Light
We can thank Thomas Edison for making modern incandescent light broadly available. Blue light, used by electronic devices including TVs, computers, mobile phones and tablets was developed and introduced in the 1990s. Unfortunately, these artificial light sources have convinced our brains that daylight is around longer than it actually is and that we need to stay awake longer than we need.
The effects of blue light exposure are particularly pernicious in that they stay long after the blue light is turned off. Dr. Walker points to a study where participants were exposed to 90 minutes of iPad usage and the “lingering aftereffect” of the blue light on brain sleepiness was several days.
Alcohol
While some people think that alcohol helps their sleep, it is actually a sedative. It puts you out but does not put you to sleep. That is why you feel groggy even though you “slept” through the night. Further, alcohol consumption has a detrimental affect on REM sleep which plays an important role in memory formation.
Dr. Walker’s advice is if you want to sleep soundly, eliminate alcohol altogether from your life. Sorry!
Ambient Temperature
Your circadian rhythm triggers a number of changes in your body throughout the day. One of these changes is the lowering of your core temperature as the day comes to end. This is a signal to the body that sleep is coming soon. As a result, your best sleep occurs when the ambient temperature is cool since this is conducive to keeping the core body temperature low.
This is something that we have had for many many years. Our long-ago ancestors lived in environments that had warm days and cool nights. Our resettlement in different parts of the planet and the introduction of innovations like central heating have potentially disrupted this ancient pattern.
Alarms, Wake Up Calls and Other Disturbances
Dr. Walker points out that we are the only “species that demonstrates an unnatural act of prematurely and artificially terminating sleep.”
The standardization of work times during the industrial revolution caused us to start our days with alarms, whistles and loud bells. Dr. Walker points out that a sudden, unexpected wake up “spikes our blood pressure” and accelerates the heart. Neither of these is good for our health. While sudden sleep termination might not the source of your dysfunctional sleep, it is certainly not good for your overall health and well being.
While a regular wake up time is seen as part of good sleep hygiene, sudden and artificial sleep interruptions should be avoided. Try to wake up at the same time each morning without an alarm clock.
Fixing Your Sleep: Medication or Therapy
Dr. Walker is no fan of sleeping medication. Repeated use can affect mortality rates and withdrawal leads to a rebound effect. He would like to see sleep medications that aid sleep but, to date, none exist.
The scientific evidence, on the other hand, supports therapy as the path to fixing sleep, specifically Cognitive Behaviour Therapy for Insomnia (CBT-I).
I’ll let Dr. Walker present the case in his own words. “So powerful is the evidence favouring CBT-I over sleeping pills for improved sleep … and so limited or nonexistent the safety risks associated with CBT-I that in 2016, the American College of Physicians made a landmark recommendation.”
This recommendation was based on an extensive study presented in the Annals of Internal Medicine. The study results stated clearly to physicians that “CBT-I must be used as the first line of treatment for all individuals with chronic insomnia, not sleeping pills.”
Conclusion to Why We Sleep
While much of Dr. Walker’s book is devoted to understanding the role of sleep and he delves into the societal issues associated with the sleep epidemic, I still believe the average sleep sufferer will benefit from this book. His explanation of how sleep works is well worth the read and will help you understand and manage your sleep problems.
Dr. Walker’s book is not only a significant contribution to our understanding of sleep and why we sleep, it has stimulated much-needed and overdue dialogue and lead to a mindset change with how we, as a society, see sleep. In fact, Bill Gates recommends Why We Sleep on his Gates Notes website.
Where to Purchase
You can purchase Why We Sleep on Amazon. Please note I receive small commission from Amazon if you purchase the book.
Exercise Recommendations for Osteoporosis
Exercise is an essential ingredient to bone health. If you have osteoporosis, therapeutic exercise needs to be part of your osteoporosis treatment program.
But what exercises should you do and which ones should you avoid? What exercises build bone and which ones reduce your chance of a fracture? Is Yoga good for your bones? Who should you trust when it comes to exercises for osteoporosis?
A great resource on exercise and osteoporosis is my free, seven day email course called Exercise Recommendations for Osteoporosis. After you provide your email address, you will receive seven consecutive online educational videos on bone health — one lesson each day. You can look at the videos at anytime and as often as you like.

I cover important topics related to osteoporosis exercise including:
- Can exercise reverse osteoporosis?
- Stop the stoop — how to avoid kyphosis and rounded shoulders.
- Key components of an osteoporosis exercise program.
- Key principles of bone building.
- Exercises you should avoid if you have osteoporosis.
- Yoga and osteoporosis — should you practice yoga if you have osteoporosis?
- Core strength and osteoporosis — why is core strength important if you have osteoporosis?
Enter your email address and I will start you on this free course. I do not SPAM or share your email address (or any information) with third parties. You can unsubscribe from my mail list at any time.
The Effortless Sleep Method by Sasha Stephens
Sasha Stephens’ book, The Effortless Sleep Method, is more of a prescription to better sleep from someone who was a chronic poor sleeper than the deep dive into sleep that Dr. Walker and Dr .Winters do in their books.
Ms. Stephens argues that sleep medications and sleep restriction therapy (SRT) are not effective because they are a crutch that inhibit the person with chronic dysfunctional sleep from getting control over their sleep.
She sees drugs as very problematic. First they are sedative and do not induce natural sleep. Second, the sleep hangover (or groggy state) that they cause coupled with sleep deprivation, create misery for their user. Third, they have a terrible rebound effect so that when the patient stops using them, the insomnia returns in a worse form than before.
Twelve Promises to Yourself
She believes that SRT is too difficult for people to follow and, as a result, most people fail. Instead Ms. Stephens recommends that people follow her program (or method) that includes twelve promises. These promises are evenly split between sleep hygiene and belief modification.
While I generally agree with her recommendations (probably because they resemble the techniques used in CBT-I), I don’t agree that SRT is perceived as a crutch by the practitioner. I agree that it is hard to complete SRT until it resets your internal sleep mechanism. However, if you practice SRT while following a strict sleep hygiene, you improve your overall chance of achieving your goal: better sleep.
If you are unable to access a qualified sleep therapist, I recommend the book solely because it does provide a clear step-by-step framework to improving your sleep. Her book was written in 2010 and is not as up-to-date or research-based as the The Sleep Solution or Why We Sleep. As a result, I would take her prescription and add some of the points made by Winters and Walker, specifically those associated with alcohol, caffeine and modern light.
Where to Purchase
You can purchase The Effortless Sleep Method on Amazon in paperback. Please note I receive small commission from Amazon if you purchase the book.
The Circadian Code
Your sleeping problems (as well as your weight and other health issues) could be caused by an out-of-rhythm circadian rhythm. In his book, The Circadian Code, Satchin Panda, PhD discusses the latest research on circadian rhythm, presents a number of surprising facts about it, and identifies ways you can get your circadian groove back to where it should be.
Dr. Panda is a leading researcher on circadian cycles and has unearthed many of the major findings regarding our circadian rhythm. He is well versed on the topic. For example, Dr. Panda was one of the researchers who discovered melanopsin — the light-sensing protein in the eye that calibrates the sleep-wake cycle from the presence of light.
While the other books presented in this post specifically address sleep and how to fix dysfunctional sleep, this book aims wider. It looks at your circadian cycle and how it affects your sleep, your weight, and your overall well being. If you want a deeper understanding of your health, I encourage you to read Dr. Panda’s book.
What is the Circadian Rhythm?
Wikipedia provides a good definition of the circadian rhythm.
“The term circadian comes from the Latin circa, meaning ‘around’ (or ‘approximately’), and diēm, meaning ‘day’. A circadian rhythm is a roughly 24 hour cycle in the physiological processes of living beings, including plants, animals, fungi and cyanobacteria.
In a strict sense, circadian rhythms are endogenously generated, although they can be modulated by external cues such as sunlight and temperature.
Circadian rhythms are important in determining the sleeping and feeding patterns of all animals, including human beings.
There are clear patterns of brain wave activity, hormone production, cell regeneration and other biological activities linked to this daily cycle.”
Dr. Panda points out in his definition that the circadian rhythm “optimizes biological functions. Every function in the body has a specific time because the body cannot accomplish all it needs to do at once.” In other words, biological functions are spread out throughout the 24 hours of the day.
Why Your Circadian Rhythm Matters
Dr. Panda opens his book with a statement: “To have rhythm, to be in sync, is to be healthy. But not just any rhythm will do.”
With this, Dr. Panda spends the remainder of the book explaining how your circadian rhythm should work and how to get it back in sync. Your circadian rhythm is the clock that sets and modulates the tone of your life and well being. Every organ, every physical activity, and every bodily function is set by your circadian rhythm. If these are out of sync, then your overall health and well-being are compromised.
In his book, Dr. Panda provides excellent resources to help you determine if your circadian rhythm is off and how to correct it.
We Are All Shift Workers
Dr. Panda provides a number of interesting insights into the circadian rhythm. The first is that all (or at least most) of us are, one way or another, shift workers.
As you likely know, shift workers work through the night and try to sleep during the day. This runs counter to the natural rhythm of our circadian clock. With that aberration, comes health problem such as early dementia, heart attacks, weight gain, and diabetes.
Dr. Panda suggests that the advent of several modern phenomenon that shift and disrupt our circadian clock make all of us, to a degree, shift workers. Examples he provides are life style changes like long work hours, jet lag from travel, and season time changes that shorten our days.
How the Circadian Rhythm Works
Dr, Panda indicates that every organism (including humans) spends its 24 hour day getting food, protecting itself, repairing itself, reproducing.
All of bodily functions are dictated by the circadian rhythm. The circadian rhythm is influenced by the lifecycle of each day. As the day becomes night, the circadian clocks in our body respond accordingly.
Dr. Panda points out that every organ has a circadian clock operating in its own time zone, activated by different stimuli.
The master circadian clock is the suprachiasmatic nucleus (SCN) in the brain (mentioned in the book by Dr. Winters). SCN is the “link between light and timing because is receives information about light from the outside world and shares it with the rest of the body.”
There are three core rhythms that influence our circadian code: sleeping, eating, and physical activity. If these are out-of-whack, so is our circadian rhythm.
When You Do Things Matters
One of the most important insights Dr. Panda makes in the book is that “when” you do things associated with sleeping, eating, and physical activity matters as much as “what” you do. This is because the “when” affects the timing of the circadian clock.
Dr, Panda wants you to “focus not so much on the what of a healthy lifestyle but on the when. A healthy lifestyle includes what and when you eat, when and how much you sleep, and when and how often you move.”
The events you should monitor are:
- When and how you wake up.
- The time you take your first bite or sip of the day.
- End of your last meal or drink.
- When you go to sleep.
- What time you shut off all screens.
- What time you exercise.
Sleep and The Circadian Rhythm
Dr. Panda points out that the combination of timing, light and food affect your sleep. He pays particular attention to the affects of light on our circadian pattern and sleep. Blue light is fine during the day, but will cause problems during the evening. As we age, our circadian rhythm weakens, so those of us of advanced age should be careful and avoid our iPhones, iPads, TVs, and high temperature lights after 6:00 PM.
Eating and the Circadian Rhythm
While light affects the circadian rhythm timing in the brain, eating affects the circadian rhythm timing in other organs. Dr. Panda states that “eating the same time every day is one of the most powerful ways to maintain a strong circadian rhythm. This is true for breakfast and dinner especially. Between these two meals, it’s less important to focus on when you eat and more important to focus on eating foods that support a healthy brain.”
Dr. Panda promotes the practice of Time Restricted Eating (TRE). His research shows that the body does not want to process food at night and instead use that time to repair and rejuvenate the body.
Time Restricted Eating (TRE) involves restricting your eating to a specific time period during the day. The optimal eating window, he points out, is between 8 and 12 hours.
Exercise and the Circadian Rhythm
Dr. Panda recommends “exercise for everyone and those with sleep disorders might find that it has a strong influence on their circadian code … They will go to sleep more quickly and wake up less often.”
Circadian Rhythm and Bone Health
Readers of this blog will be interested to know that the circadian rhythm has a direct influence on bone heath and osteoporosis. Here is a summary several key developments.
Insights into the Role of Circadian Rhythms in Bone Metabolism
In a study publish in 2018 in BioMed Research International, Chao Song and others state “disruption of the circadian clock due to shift work, sleep restriction, or clock gene knockout is associated with osteoporosis or other abnormal bone metabolism, showing the importance of the circadian clock system for maintaining homeostasis of bone metabolism.” (3)
The authors’ make the following conclusions:
- Bones are organs under dynamic regulation of osteoblasts, osteoclasts, osteocytes, and bone lining cells. Disruption of the balance between these cells leads to diseases such as osteoporosis.
- Increasing evidence demonstrates that the circadian clock systems, including the master pacemaker and peripheral circadian machinery, play pivotal roles in maintaining homeostasis of bone metabolism.
- Circadian disruption due to sleep restriction, shift work, fasting, or knockout of clock genes results in disrupted homeostasis of bone metabolism.
- [There is] evidence that the circadian system may be a promising target of clinical intervention for abnormal bone metabolism.
Dr. Panda’s Position on Circadian Rhythm and Osteoporosis
I’ll let Dr. Panda explain the relationship between bone health and circadian rhythm in his words.
“With regular wear and tear, bones go through a daily repair process. Our bones are made of minerals, including calcium, that are secreted by cells. Another type of bone cell eats up damaged bone; the circadian clocks in these cells are synchronized so that bone eating and bone making do not occur at the same time of day.
The balance between these two cell types is important. Too much bone eater cell activity can lead to bone loss, while too much bone making can push against the other bones and create additional damage near joints.
As we age or when our lifestyle is erratic, our circadian clock gets weaker. When this happens, the bone-making cells are not fully activated every day, so they don’t produce enough raw materials for making new bone. Similarly, the bone-eating cells are not fully activated, so they don’t clear all the damaged bone material completely. This ultimately leads to weaker bones that are prone to fracture. To maintain the healthiest bones, we need to have a strong sleep-wake cycle, eat at the right times, and exercise.”
Conclusion to The Circadian Code
The current research indicates that there are substantial benefits, including bone health, to getting your circadian rhythm in good operating form. While the researchers know the benefits, there is still work to be done on how to get one’s rhythm back.
If you are dissatisfied with your sleep and you are concerned about your bone health, you should consider how well you are managing your circadian cycle. Are you respecting your natural time and pace? To learn more, I encourage you to read Dr. Panda’s book.
Where to Purchase
You can purchase The Circadian Code on Amazon in paperback. Please note I receive small commission from Amazon if you purchase the book.
Best Sleep Training Books Summary
If your sleep is broken you should fix it. The health benefits are considerable. My conclusion after reading these sleep training books is that changing your nightly sleep from dysfunctional to natural is essential to your well being and should be a priority.
I also learned that sleep is something we were given and is, by default, a natural occurring daily event. Daily habits disrupt that natural cycle. Thoughts and anxieties about our sleep only make a difficult situation worse.
To fix our sleep, we will likely have to change our mindset and established patterns that disrupt our sleep. For example, the brain is an association machine and if we regularly read in bed, then our brain will associate our bed with reading time and diminish its association with the sleeping event. As a result, we should restrict our time in bed to sleep only and not any other activity (sex is the exception to this rule.)
Steps to Fix Your Sleep
Here is a quick summary of how to fix your sleep from the sleep training books reviewed in this article:
- If you think you have a sleep problem, consult with your physician and request a sleep assessment.
- Sleep medications do not work. They make a bad situation worse because of the grogginess they cause and the rebound effect when you withdraw the medication.
- Cognitive Behaviour Therapy for Insomnia (CBT-I) is the route to better sleep. It requires that you:
- Understand your sleep.
- Eliminate bad sleep habits.
- Follow proper sleep hygiene rules.
- Reduce your anxiety towards your sleep.
- Follow the sleep restriction therapy (SRT) protocol for a period of time to reset your internal clock and calibrate how much sleep you really need.
The challenge for most of us is finding the right resources, support and guidance to fix problem and not fall off the wagon. These sleep training books are a great start and, depending on your commitment and motivation, might be your path to great sleep. The rest of us should find a trained sleep professional who can lead us to the joy of a regular good night’s sleep.
References
- Ochs-Balcom et al. Short Sleep Is Associated With Low Bone Mineral Density and Osteoporosis in the Women’s Health Initiative. Journal of Bone and Mineral Density. 06 November 2019.
- Aspelund, et al. A dural lymphatic vascular system that drains brain interstitial fluid and macromolecules. Journal of Experimental Medicine, 29 June 2015. 212(7): 991
- Choa Song, et al. Insights into the Role of Circadian Rhythms in Bone Metabolism: A Promising Intervention Target? BioMed Res Int. 2018. Published online 2018 Sep 27. doi: 10.1155/2018/9156478

Comments
January 22, 2019 at 3:57pm
Peggy B.
Hi, I found this review interesting and may read the book. I would also like to put a plug in for another book, written by an insomniac, that helped me a lot with my sleep problems. “Desperately Seeking Snoozin’” was recommended by a respirologist in Ottawa who I saw after going to the sleep clinic at the Ottawa Hospital. In fact, she had bought dozens of copies of the book and gave it to everyone who came to her for sleep problems.
The book is folksy and may get on your nerves occasionally but it was written as an act of love by John Wiedman, a self-cured insomniac who wanted to help others. It was my bible for a number of months and I still refer back to it when I hit a bad spell and can’t sleep for awhile. It is available on Google books and maybe elsewhere too.
He also prescribes the identical cure as discussed in this review, of limiting hours of sleep by determining the minimum you need to get by (I had to stay up til 1 a.m.) and getting up at the same time every day. This was accompanied by keeping a sleep diary and preceded by writing a sleep biography to try to determine one’s problems. I no longer need to keep such strict sleeping hours, but I did do so for many months.
I am glad to hear there is another, more scientific book out there and will share this review with other friends. All the best,
Peggy B.
January 22, 2019 at 4:07pm
Richard Martin replies
Hi Peggy: Thank you for your comments and sharing the book that you found useful.
January 22, 2019 at 6:48pm
Renee V
I have a question about the book. With regards to sleep apnea, does the author merely repeat the usual "CPAP is the gold standard," "try a dental device if you can't tolerate CPAP," "lose weight (if applicable)," etc. or does he have any novel suggestions for treatments?
January 23, 2019 at 10:31am
Richard Martin replies
Hi Renee: I did not cover sleep apnea in my review because it, as you point out, requires a much different treatment protocol.
Dr Winters does discuss sleep apnea in chapter 14 and some of the interventions available. He points out that continuous positive airway pressure (CPAP) is the most popular treatment option. The other treatment approaches he mentions are 1) sleeping on your side, 2) oral appliances, and 3) surgery - which can be as easy as a tonsillectomy or as complex as a reset of the jaw. He does mention newer surgical options.
I recommend you consult with a sleep specialist if you have sleep apnea.
January 22, 2019 at 10:41pm
Megan
So excited to learn of The Sleep Solution. I am arguably one of the healthiest people in my circle -- a girl with a quality diet, regular exercise regime, fulfilling work/social life, etc -- but my missing piece has always been SLEEP. Insomnia has plagued me for 6 years for reasons unknown. The media and medical field have indeed added shame to the the issue... minimizing the gravity of unrest. "Try a hot bath and warm milk -- that should fix things". Their oversimplification of the matter is insulting.
Sleep is such a fascinating, delicate, and underappreciated event. A true quality of life issue.
I'm compelled to buy the book... Most grateful for this review and post.
January 23, 2019 at 10:03am
Richard Martin replies
Hi Megan: Thanks for your comments. I agree that many of the articles you read on the web simplify the solution too much. Dr. Winters' book provides the education and points to several viable solutions. Well worth the investment!
January 23, 2019 at 8:00pm
Renee V
Thanks for your reply. I've already consulted with a sleep specialist who diagnosed me. All treatment options have been intolerable and/or ineffective. Even explored surgical options with a different doctor - don't really qualify for surgery as considered to be "mild" even though I am tired and fatigued continually. I sometimes have some of the other sleep issues and rarely get more than 6 hours sleep max, although I do sleep. Fibromyalgia related sleep architecture anomalies may also be contributing. Thanks for your book review.
January 24, 2019 at 9:24am
Richard Martin replies
Hi Renee
I am sorry to hear that you are "sleep challenged". It must be frustrating. Thank you for your kind comments.
January 24, 2019 at 4:11pm
Phyllis Morris
Thank you for your review, Richard. The Sleep Solution is on my reading list for future. Right now, I'm busy trying to help my 91-year-old mother. She still gets around but has a horrible time sleeping through the night. Does Dr. Winter discuss age-related changes in sleep patterns? Does he address situations such as overactive bladder? I agree whole-heartedly with his take on trazadone. I think it's overused due to its affordability for mental health treatment. Any thoughts are greatly appreciated! Sincerely, Phyllis M.
January 24, 2019 at 4:54pm
Richard Martin replies
Hi Phyllis:
Thank you for your reading the post and your kind comments.
In his book, on pages 31 to 34, Dr. Winters discusses how much sleep we need and delves into how our sleep needs change as we age. He refers to research, done in 2014 and published in 2015, that examined sleep needs among nine different age groups. The study found that the amount of sleep we need declines as we age to the point where our elders only need seven to eight hours a night.
When asked how much sleep we need, Dr. Winters responds: "Enough". Not too little and not too much. I suspect if you were to ask him about your 91 year old mother, putting aside obstructive sleep issues like apnea, he would recommend the protocol I followed.
He did not discuss overactive bladder as an issue; at least I could not find it. However, he does discuss antihistamines and their effect on dementia; as well as a medication to treat overactive bladder, oxybutynin, as another potential cause of dementia.
Dr. Winters is no fan of medications as an answer to your sleep problems. He is a believer in you finding out about your sleep, how much you need, regulating your sleep and sticking to a schedule.
If overactive bladder is an issue, you might want to consult a pelvic health Physical Therapist. They have tricks and strategies that can help you address this issue and not interrupt your sleep.
If sleep is a concern for you I highly recommend Dr. Winters' book largely because you will learn a lot about your sleep and he helps to eliminate much of the poor quality information available on the internet (not ours, of course!).
March 11, 2020 at 9:20am
Nora James
i too suffer from urgency of micturition and an overactive bladder. I have noticed that I am often woken up with a full bladder and then find it difficult to get to sleep again. I take medication for this and have seen a bladder specialist nurse. i live in the UK and I am in my eighties. Do any of the sleep specialists give any space in their books to this problem?
March 11, 2020 at 2:33pm
Richard Martin replies
Hi Nora. Thanks for contacting us and your question. Sorry to hear about your predicament. I recall Dr. Winters mentioning the situation in his book but there was no further discussion. This is something you should best discuss with your physician.