Table of Contents
What is it like to live with a compression fracture? Are there effective ways to treat a compression fracture with Physical Therapy? Do I recommend specific exercises for my clients with compression fractures? Is there a best way to sleep with a compression fracture? I answer each of these questions in this blog post.
In the video, you will meet Brenda — one of my clients with compression fractures — and hear her story of how her compression fractures happened, how they affected her quality of life, and what she has done to return to living an active life.
The first video, is 25 minutes long. There are two more videos later in the blog. One is 5 minutes in duration and the other is 10 minutes. If you are at risk of a compression fracture, already have one or know someone suffering from a compression fracture, you should read this blog post and view the videos — the time you invest will be well worth your while. I promise.
Introduction
My patient, Brenda, is here to share with you how her life has been impacted by compression fractures.
Of all the individuals that I’ve worked with who have compression fractures, Brenda is the most positive and persistent client. She does every single compression fracture exercise I ask her to do. Each time we meet she arrives with her completed checklist and asks me questions specific to compression fractures.
When Brenda prepared for today’s talk, she realized how frustrated she was with her situation. She felt despair and anger because of her compression fractures. I asked her not to emphasize her frustration but, instead, share the tactics that have helped her deal with her compression fractures. Brenda’s story is meant to help all of those individuals, men and women, with compression fractures who are suffering in silence.

Brenda’s Thoracic Compression Fracture
Brenda is a retired teacher. She has always enjoyed gardening, bi-weekly exercise classes, and daily walks.
In her thirties Brenda realized that she needed to look after her bones. Her mom had fractured both of her hips as well as her pelvis. Brenda’s genetics and family history of osteoporosis were red flags indicating that she might have some issues with her bones sometime in the future.
A routine DEXA (Dual-Energy X-ray Absorptiometry) test and FRAX score, in 2011, showed that Brenda had some bone loss. She was diagnosed with osteopenia. She became more careful, watched the calcium in her diet, her vitamin D levels, and continued her exercise classes.
Her General Practitioner recommended bisphosphonates, but she couldn’t tolerate them. He switched her to Prolia. She was on Prolia for four years. A repeat DEXA showed that she had improved, so she discontinued her Prolia injections in the spring of 2015. She was excited because she felt she had turned the corner. Brenda concluded that her bones were healthy because of her exercises, diet and Prolia injections. It turned out that Brenda came to this conclusion prematurely.
T9 Compression Fracture
Once she got the clean bill of health, Brenda planned a dream holiday for her and her husband — a five week trip to Africa.
Unfortunately, that dream holiday became a nightmare. On the first day of the trip she experienced severe back pain (read this post to answer the question: can osteoporosis cause back pain?) when she moved some heavy bags. She was able to manage the pain because she had some over-the-counter pain medication with her. However, by the time the trip ended, she was in severe pain. Too severe for her pain medications to suppress. The more potholes she hit as they drove across Africa, the worse her pain got.
As soon as she returned to Canada, she went to see her doctor. He diagnosed her with a strained back. Unfortunately, a series of x-rays showed that Brenda had a 70% T9 compression fracture. It was a thoracic compression fracture and four other vertebrae had some level of compression.
Physical Therapy Treatment for a Thoracic Compression Fracture
I asked Brenda to discuss the treatment she received after the diagnosis of her compression fractures.
After the diagnosis of compression fractures, Brenda was given strong painkillers that helped manage the pain and allowed her to sleep. The physiotherapist (the one she saw before she came to see me) helped with the pain. The physiotherapist used hot pads, electrical pulses that stimulate the muscles, acupuncture, and a minimal amount of ultrasound. That initially helped with the general pain.
Can You Make a Compression Fracture Worse?
I wish more people asked me this question because so many people don’t realize that yes, your vertebral fracture can get worse.
It is so very important to remind yourself that this can happen.
How you get up in the morning, how you choose to move a certain way, how you dress, how you tie your shoes, how you garden – all of those things allow you to be in control and avoid your compression fracture to become more compressed.
If you currently have a 30% compression of your vertebral body, it can become 40% or even 50% compressed.
Some people can compress their vertebral body so much that they can’t see it on an x-ray anymore. It is not something I wish on any of you.
However, since you’re watching this, this is likely not to occur because you’re taking things in hand and you’re empowering yourself to be able to move well.
I asked Brenda if either the physician that gave her the diagnosis or the initial physiotherapist who treated her told her that the compression fractures could get worse by how she moved.
Brenda said she was not informed about this. In fact, she did not even know that one of her compression fractures, a T9 compression fracture, was compressed 70% and could not be fixed.
I find that many people do not understand the importance of good posture, good movement and the potential repercussions on the health of their spine. I encourage readers to read my blog post on Osteoporosis Posture Explained where I discuss, in detail, key concepts related to postural alignment and how good posture practices can fend off compression fractures.
How to Move When You Have a Compression Fracture
Compression fractures are not static. How you move throughout the day, the exercises you do, how you lift, how you bend, how you get in and out of bed — all of these things can either keep the vertebra from becoming more compressed or cause further collapse. This is not meant to scare you. Rather, it is meant to inform you that it is in your control to help yourself reduce the further risk of a compression fracture.
Vertebral Kyphoplasty and Compression Fracture
A surgical technique called vertebral kyphoplasty would be the only way to fix her T9 compression fracture. This intervention would have to happen within the first six to eight weeks after a T9 compression fracture. During a a vertebral kyphopasty surgery, the surgeon re-inflates the vertebra with kyphoplasty and then injects a form of cement into the vertebral body.
Although a vertebral kyphoplasty can give you pain relief, it doesn’t actually stop the progression of further compression fractures. The importance of good body mechanics and diligence during your exercises is really important — despite having that type of intervention.
Further, the vertebral kyphoplasty could be detrimental because it could make one strong section with weaker bones around it.
Exercise Recommendations for Osteoporosis
Exercise is an essential ingredient to bone health. If you have osteoporosis, therapeutic exercise needs to be part of your osteoporosis treatment program.
But what exercises should you do and which ones should you avoid? What exercises build bone and which ones reduce your chance of a fracture? Is Yoga good for your bones? Who should you trust when it comes to exercises for osteoporosis?
A great resource on exercise and osteoporosis is my free, seven day email course called Exercise Recommendations for Osteoporosis. After you provide your email address, you will receive seven consecutive online educational videos on bone health — one lesson each day. You can look at the videos at anytime and as often as you like.

I cover important topics related to osteoporosis exercise including:
- Can exercise reverse osteoporosis?
- Stop the stoop — how to avoid kyphosis and rounded shoulders.
- Key components of an osteoporosis exercise program.
- Key principles of bone building.
- Exercises you should avoid if you have osteoporosis.
- Yoga and osteoporosis — should you practice yoga if you have osteoporosis?
- Core strength and osteoporosis — why is core strength important if you have osteoporosis?
Enter your email address and I will start you on this free course. I do not SPAM or share your email address (or any information) with third parties. You can unsubscribe from my mail list at any time.
Brenda’s Life Before Her Vertebral Compression Fractures
Brenda’s vertebral compression fractures changed her lifestyle. She states that her life went from “white to black” — a 100% change in her life. Here she details each of the parts of her life that have been affected by her compression fracture and how she has had to accommodate the pain from the compression fracture.
Community and Family Activities
Before the compression fracture, Brenda was the “Energizer bunny”. She was involved in the community association, university women’s group; did things at home like refinishing furniture for her daughter; and was engaged in lots of activities.
But all that changed 100% because of the pain.
Gardening
Brenda has had to hire young women to help her with the garden because gardening involves hauling, lifting, heaving, and shovelling. These activities can be bad for your back when done incorrectly. All she can do now is deadhead plants. Gardening was a stress reliever before, now it’s a source of stress.
Cleaning
Brenda considers herself to be one of those “odd people” that likes to clean. Again, it’s sort of a feel good thing, but she has had to hire a cleaning lady to help her with the heavy stuff, the vacuuming, the washing of floors, the toilets — all those things that put extra strain on her back.
Laundry
Brenda can do a little laundry, but ironing is very difficult, so she has embraced the “rumpled linen look”.
Driving
When she first had her T9 compression fracture, Brenda could not drive. She could hardly get into the car when she had to go to various appointments. It has only been of late that she feels comfortable enough to drive, but she is much lower now in the seat of the car — three inches lower. It took nine months from the time of the initial severe pain to get to the point where she can drive again.
Food Preparation
Brenda’s husband has health issues of his own and he is very limited in what he can do. In the beginning, shortly after the compression fracture food preparation was limited to semi-prepared or prepared foods.
Brenda is limited in what she can do in the kitchen. For example, in order to peel a potato or a carrot, she had to put both my forearms on the counter. She could not lift a dish in or out of the oven.
Grocery Shopping
Brenda is unable to do the grocery shopping and has left that task to her husband.
General Mobility Around the House
Brenda had to use a walker for the first time ever in her life after the compression fracture. She used it to get out of bed and to the bathroom in the morning. She has not had to use a walker for about the last three weeks.
Clothing
Brenda has had to “embrace the crumpled look” because everything hurts around her middle. She finds that she cannot wear tight clothing that might press on the bone that is protruding in her back.
Physical Therapy Treatment for Vertebral Compression Fractures
The following are the compression fracture Physical Therapy treatment modalities that helped her with her compression fracture.
Myofascial Release Therapy for Compression Fracture
Brenda indicated that the best compression fracture Physical Therapy treatment option for her has been myofascial release. It has helped with the initial spasms. She experienced really bad vice-like grips around her right hip after an episode with the spasms. These have been taken that away completely.
Also, because the tightness in her chest has been reduced, she feels a little bit more erect. She does not have that same pulling forward sensation that she experienced before.
Targeted Compression Fracture Stretching Exercises
Brenda never lets a day go by without doing her targeted stretches. She finds them to be really helpful. They relieve her pain or her aches. They help her with fighting this gravitational pull that she experiences from morning till night.
Brenda does stretches from the Exercise for Better Bones program but I have advised her to hold them a lot longer (as long as 10 minutes) than I have recommended in the book. They are more like a fascial stretch.
Brenda finds that it takes the 10 minutes for her body to release and relax into the stretch. She finds that the prolonged fascial stretches make her feel good.
Dynamic Taping for Compression Fracture
Brenda finds the dynamic tape to be another kind of little miracle worker. She could not believe that it actually works. When it’s not there, she can really feel the difference. It has really helped with that long muscle in her back that is strained.
Strengthening Exercises for Compression Fracture
Brenda finds the strengthening exercises to be very beneficial. Because she was physically fit before the compression fracture, her muscle memory is coming back. Every time she improves in her exercises, her muscles are activated; and every time those muscles are activated, she is stronger in whatever she does, whether it’s getting off the toilet, getting out of a chair, getting out of bed in one smooth motion. This is a big, big step and improvement for Brenda.
Be Fit Before Your Compression Fracture
There are considerable benefits to being fit before the compression fracture. Unfortunately, a lot of women and men do not exercise until something happens and their body does not have a positive association with exercise. Brenda did.
As a result, Brenda was used to muscle soreness from vigorous exercise. Women and men who have not exercised before think that something has gone wrong. Brenda has always had a positive association with exercise. I think that is very important. I encourage listeners to exercise in a regular basis.
Strengthening Exercises
Brenda found the strengthening exercises that I have given her to be initially were very hard to do even though she was fit. She could hardly lift my head up off the floor. But, to her credit she did one rep, and then she did three reps, and then she did 5 reps, and then, eventually, she did 10 reps.
Brenda considers it “baby steps” progress. She is fastidious about her chart and can see her progress. She finds this motivating. If you understand intellectually what the exercise will do, then she really motivated in terms of her everyday life. So that really, really has helped.
Nordic Walking with Weighted Kypho Orthosis Vest
Brenda uses activator poles (Nordic walking poles) with a weighted kypho-orthosis vest. She used to walk five kilometres plus a day. After the compression fracture the most she could walk was five houses and back — and that exhausted her.
Today she is up to three kilometres walk at a snail’s pace. She can do it with the poles and the vest because it keeps her in the proper position.
The weighted kypho-orthosis vest helps her walk more upright because it counterbalances the weight of her head and allows her to control where her posture is taking her. She is also wearing the weighted kypho-orthosis vest when she prepares her meals.
Brenda says the vest helps her stay more upright because her body naturally wants to go forward. That’s the go-to position and she has to fight that all the time.

Advice for Your Younger Self
I asked Brenda knowing what you know now, what would you tell your younger self? Here are Brenda’s thoughts on that question.
Choose the Right Health Professional
The first thing she would tell her younger self (in fact, what she has told her daughters) is that you have to be really fastidious, as much as you can be, about choosing your general practitioner, or your family doctor.
He or she should be your strongest advocate in the medical system. They should listen carefully, they should be able to communicate well to you, so that if you don’t understand the medical jargon that they break it down for you. They should be able to answer the questions you have and anticipate the questions that you don’t have — the things that you should know.
Be Assertive and Own Your Health
You may have to be assertive to get your needs met. For Brenda that’s not such an easy thing to do. But one has to stand up for one’s rights and it’s their professional duty to find out if they don’t know. And they won’t know everything. Often your physician is a generalist. But they do have a professional obligation to find out and to send you on to a specialist who does know.
Keep a Copy of All Tests
You should keep a hard copy of all tests that you have even in this day and age of electronic copies. Have a file so that you can trace back your health history. It will save a lot of time.
Take Someone With Your When You Are in Severe Pain
When you are in really severe pain, you need to take somebody with you to the doctor because the brain is fuzzy under pain and you just are not fully aware of what is happening.
Get a Second Opinion
Brenda says you should not be afraid to get a second opinion. It doesn’t hurt. The world is not going to fall apart. If it doesn’t feel right, it probably isn’t right. You know your own body, and that is important to follow through.
Pay Attention to Your Diet
Be bone health aware in terms of not just milk, but other sources of calcium as well. Especially after you have left home. You have to be your own calcium conscience.
Exercise
Get fit and exercise. But, Brenda was not aware of the kinds of exercises that were detrimental to her spine. Many fitness professionals are not trained to deal with a person with osteoporosis. Brenda did the wrong exercises with gusto. She is now paying the price.
Back Brace for Compression Fracture
In this section we cover how to choose a back brace for compression fracture and discuss Brenda’s experience.
Understanding Back Brace for Compression Fractures
A back brace for compression fracture is a supportive device designed for individuals who have sustained one or more vertebral compression fractures.
These braces provide targeted support for either the lumbar spine (the five vertebrae in the lower back) or the thoracic spine (the 12 vertebrae in the middle back where the ribs attach). The specific type of brace depends on the location and severity of your compression fracture.
Types of Back Braces for Compression Fractures
Selecting the appropriate back brace for compression fractures requires careful consideration of two critical factors.
- First, you must identify the exact location of your vertebral compression fracture to ensure the brace supports the affected area of your spine.
- Second, you need to determine the level of support or rigidity required based on your fracture’s severity.
For minimal compression fractures, very little support may be needed, and some individuals may not require any brace at all. Many people with compression fractures experience no pain and can heal naturally without additional support.
However, if you’re experiencing significant pain or your orthopedic physician has determined that your compression fracture is unstable, a more rigid back brace for compression fractures will be necessary. In these cases, your physician will recommend the appropriate level of stability needed to keep your spine safe during the healing process.
Choosing the Right Back Brace for Your Compression Fracture
The selection process begins with identifying the precise location of your compression fracture. Your back brace must provide stabilization and support specifically around the fractured area.
The choice largely depends on how fragile and vulnerable your compression fracture is—if the fracture is severely compressed and causing nerve irritation, you’ll likely need a brace with greater stability and rigidity.
Professional guidance is invaluable in this selection process. Ideally, you should work with a physical therapist trained in back brace fitting for a compression fracture or an orthotist who specializes in spinal support devices.
It’s worth noting that very few orthopedic surgeons routinely recommend back braces for compression fractures—my observation is that only about 10% of individuals with compression fractures receive brace recommendations. This makes professional guidance even more crucial for selecting the most appropriate device for your specific condition.
Spinomed Back Brace
I recommend the Spinomed Back Brace for my clients with compression fractures. It is the only back brace that has been studied for this population.
Professional Fitting and Customization
Professional fitting is essential, especially if you’ll be wearing the brace for extended periods or relying on it for daily activities. A properly fitted back brace serves four critical functions:
- Providing enhanced stability.
- Managing pain.
- Optimizing posture and alignment for proper healing.
- Minimizing irritation to surrounding tissues.
When you’re depending on a back brace for several hours daily over an extended period, customization becomes particularly important. A professional fitting ensures the brace performs optimally while maximizing your comfort and mobility.
Duration and Proper Usage Guidelines
The duration of back brace wear depends significantly on whether your brace has been professionally fitted and customized. If you’re using a non-fitted, off-the-shelf brace strictly for support, limit wear time to activities where you specifically need additional stability—such as transferring in and out of bed, gardening, or caring for grandchildren. Avoid wearing an uncustomized brace during other activities, as prolonged use can weaken your core stabilizing muscles rather than strengthen them.
For long-term healing, the goal is to gradually transition from brace dependence to natural muscle support. Once your physician gives permission to begin core strengthening exercises and you feel your deep core muscles becoming stronger, start weaning yourself from the brace during specific activities. Your abdominal and core muscles are designed to function as your body’s internal back brace, providing natural stabilization.
If you find that your core musculature never fully develops the necessary strength, continue using the back brace minimally—only for specific high-demand activities that require additional spinal stabilization, similar to how bodybuilders use back braces for heavy lifting.
Support for L1 and T12 Compression Fractures
Compression fractures in the L1 or T12 vertebrae require special consideration due to their location at the junction between the lumbar and thoracic spine. A standard short lumbar brace will not provide adequate support for fractures in these areas. You’ll need a longer brace that extends from the lower lumbar region through the upper thoracic area.
The Spinomed brace is one example of a device that provides comprehensive support through the entire spine, making it suitable for fractures at this critical transition zone.
Why Amazon Isn’t the Best Option for Compression Fracture Braces
Purchasing a back brace from online retailers like Amazon is not recommended for compression fractures due to several significant limitations.
- First, these braces are not fitted to your specific body dimensions and spinal anatomy.
- Second, without professional guidance, you cannot determine whether a particular brace is appropriate for your specific type and location of compression fracture.
- Third, there’s no way to verify that an online purchase provides the exact level of stability and support your condition requires.
Instead, seek care from a local orthotist who can offer a variety of braces for you to try and provide personalized recommendations. You can also obtain referrals through your physician or an orthopedic specialist who can recommend the most appropriate brace for your specific compression fracture pattern and ensure proper fitting when necessary.
Real-World Experience: Brenda’s Back Brace Journey
Understanding how back braces work in practice can be helpful when making your own decision. Brenda, who has experience with compression fractures, has tried three different types of braces throughout her recovery journey, each serving different purposes and offering varying levels of support.
The Weighted Kypho Orthosis Vest
Brenda’s first brace was a Weighted Kypho Orthosis vest, specifically designed to counterbalance the weight of heavier breasts or forward head posture—common issues that can exacerbate compression fracture symptoms. She found this vest particularly helpful during walking, food preparation, and any activities requiring prolonged standing. The weighted design helped improve her posture and reduce strain on her fractured vertebrae.
Unfortunately, this specific brace has been discontinued and is no longer available through official channels. While there are products on Amazon using similar names, they do not follow the same research-based protocols regarding weight distribution and placement that made the original effective. For this reason, these alternatives cannot be recommended as suitable substitutes.
The ObusForme Back Brace
When Brenda’s back pain was at its worst during the early stages of her compression fractures, she purchased an ObusForme Back Brace from a medical supply store in Ottawa. This belt brace provided her with a sense of stability and support, making her feel like it “held things together” during her most challenging days. She would wear it specifically on days when she felt weaker or needed extra support, finding it particularly helpful during her acute pain phase.
I usually do not recommend this type of belt for most compression fractures as it might not be sized properly and, as a result, provide enough stability around the compression fracture for many people.
The Basic Lumbar Support
Brenda’s third brace was a standard lumbar support device, which unfortunately did not meet her needs. She found it lacked adequate firmness and didn’t provide the specific support her compression fractures required. The brace was not particularly supportive for her condition, and she eventually gave it to a friend, indicating that it didn’t offer sufficient benefit to warrant continued use.
Lessons from Brenda’s Experience With Back Braces for Compression Fracture
Brenda’s journey illustrates several important points about back brace selection.
- First, different braces serve different purposes—what works during acute pain phases may not be suitable for long-term support.
- Second, the specific design and construction quality matter significantly; generic lumbar supports may not provide adequate support for compression fractures.
- Finally, professional guidance and medical supply stores often offer better options than generic online purchases.
Making an Informed Decision About Back Brace for Compression Fracture
When dealing with a compression fracture, remember that not everyone requires a back brace. The decision should be based on your specific symptoms, fracture severity, and overall treatment plan. If you’re experiencing significant pain, have been told your fracture is unstable, or need additional support during daily activities, a properly fitted back brace for compression fracture can be an invaluable tool in your recovery journey.
The key to successful brace use lies in professional guidance, proper fitting, and understanding that the brace is typically a temporary support system. Your ultimate goal should be to strengthen your natural core muscles to provide long-term spinal stability.
Work closely with your healthcare team to determine if a back brace is right for you, and if so, ensure you receive proper guidance on selection, fitting, and usage duration to maximize your healing potential while maintaining your overall spinal health.
Lumbar Support Brace for Lighter Work
Brenda has a smaller lumbar brace that she wears for household things like dusting or doing the laundry.
It is not so much as a support, as a reminder: “Don’t do bad moves.” (Brenda uses the Obusforme Brace in the illustration.)
Lumbar Support Brace for Lighter Work
Brenda has a smaller lumbar brace that she wears for household things like dusting or doing the laundry.
It is not so much as a support, as a reminder: “Don’t do bad moves.” (Brenda uses the Obusforme Brace in the illustration.)
Weighted Kypho Orthosis Vest
Brenda uses a Weighted Kypho Orthosis Vest for walking, while preparing her food and any activity anything where she is standing around a long time.
The other day, while her house cleaner does all the challenging stuff, Brenda wore the vest to dust. It’s a reminder to keep upright.

Nutrition and Compression Fractures
In this section we will cover the nutrition advice Brenda follows to reduce the pain associated with her compression fracture.
Nutrition and Protein
Earlier Brenda recommended that people make sure calcium be part of their diet. While calcium is important, you should make sure you have adequate amounts of nutrients including vitamin D, magnesium and vitamin K.
Prunes have been shown to play an important role in bone health.
I find that many of my clients do not have enough protein in their diet. Protein is one of the main building blocks. If you have the protein, which is acidic, make sure you increase you intake of fresh fruits and vegetables which are alkaline and help balance the acidity in protein.

Support Devices for Compression Fractures
Heat Pad
Brenda uses a heating pad a lot. When she starts to feel achy, she sits down for 15 minutes and puts it on. It helps take the ache away. When she does her stretching exercises, she has it underneath her as well.
Reacher
The reacher is a terrific little device. It was very handy in the initial stages because everything seems to drop when you don’t want it to drop. You can use one for the garden for picking up things like sticks.
Shopping Cart
When Brenda goes to the large shopping stores, she will lean on the cart handle to take some of the pressure off her back. Sometimes she will put her purse in her back and adjust it so it is in the small of her back. It operates like the weighted kypho orthosis vest mentioned earlier in this blog post.

Lumbar Compression Fracture Exercises
Before we begin, I have a video that addresses many people’s concerns about starting an exercise program after a compression fracture.
The following are 15 the lumbar compression fracture exercises I recommend for my Physical Therapy clients with osteoporosis:
- Chest stretch
- Chin tuck
- Arm lengthening or reach back
- Arm pull back
- Shoulder Stabilization
- Abdominal activation
- Wall push-ups
- Bridging
- Prone leg lift
- Squats
- Step ups
- Bicep curls
- Horse Stance
- Floor M
- Reverse Fly
These exercise choices are based on a study published in BMC Musculoskeletal Disorders by Bennell. These can be broken into two major groups: one set of exercises for posture and flexibility and the other for strengthening. I explain these in more detail below.
I do not recommend that every one with a compression fracture do all of these exercises. Everyone is different and the exercises will need to be broken into groups and delivered at apace that works for you.
The best thing you could do is to work closely with a Physical Therapist who is knowledgeable in the treatment of compression fractures.
If that person is not accessible, then I recommend you start with the Posture Exercises outlined in my book, Exercise for Better Bones.
The Bennell study (2) looked at the effects of compression fracture exercises and manual therapy on physical impairments, function and quality-of-life in persons with osteoporotic compression fractures. The study concluded that there are positive benefits of physical therapy prescribed compression fracture exercises for patients with compression fractures.
Spine Fracture Treatment Exercises and Thoracic Compression Fracture Exercises
The exercises I have listed are appropriate as spine fracture treatment exercises and thoracic compression fracture exercises.
Physical Therapy Compression Fracture Treatment Guidelines
The following is the treatment protocol I use (based on the Bennell study) for clients with compression fractures.
Once your muscles have started adapting to the change in height caused by the spinal compression fracture and the compression fracture has had time to heal (usually 8 to 12 weeks after the episode of increased pain) you should start a compression fracture exercise program.
The goals of compression fracture exercise program are to:
- Decrease your pain at rest and with movement.
- Increase your standing tolerance and overall strength.
- Reduce your risk of falling.
I recommend that you invest time and understand how compression fractures occur and learn how to avoid all activities and postures that can make your compression fracture worse. Both of these items are covered in this blog post and in the Exercise for Better Bones program.
Physical Therapy Compression Fracture Treatment Guidelines
The following is the treatment protocol I use (based on the Bennell study) for clients with compression fractures.
Once your muscles have started adapting to the change in height caused by the spinal compression fracture and the compression fracture has had time to heal (usually 8 to 12 weeks after the episode of increased pain) you should start a compression fracture exercise program.
The goals of compression fracture exercise program are to:
- Decrease your pain at rest and with movement.
- Increase your standing tolerance and overall strength.
- Reduce your risk of falling.
I recommend that you invest time and understand how compression fractures occur and learn how to avoid all activities and postures that can make your compression fracture worse. Both of these items are covered in this blog post and in the Exercise for Better Bones program.
Physical Therapy Exercises for Compression Fracture
I recommend a compression fracture exercise program that includes a combination of postural, flexibility, strength and trunk control exercises. The specific exercise mix is dependent on the individual needs of my clients and I choose what is appropriate after an assessment.
Daily Postural and Flexibility Lumbar Compression Fracture Exercises
Each of these compression fracture exercises can be found in Exercise for Better Bones. I decide the appropriate mix of postural and flexibility exercises based on my assessment of the individual.
- Chest stretch
- Chin tuck
- Arm lengthening or reach back
- Arm pull back
- Shoulder Stabilization
With time I encourage you to progress the chest stretch by lying on your back over a rolled-up blanket. Place the blanket lengthways.
Straighten your arms out at the height of your shoulders (shown in Stronger Bones Stronger Body workout video) to open up your chest wall and reduce the constant forward pull into gravity.
Strength and Trunk Control Lumbar Compression Fracture Exercises
A selection of these compression fracture exercises can be done up to three times per week. I decide the appropriate mix of strength and trunk control exercises based on my assessment of the individual.
- Abdominal activation
- Wall push-ups
- Bridging
- Prone leg lift
- Squats
- Step ups
- Bicep curls
- Horse Stance
- Floor M
- Reverse Fly
Finally, I encourage you to work with a health care professional who can provide soft tissue massage, postural taping, or taping and gentle spinal mobilization.
Physical Therapy Exercises for Compression Fracture
I recommend a compression fracture exercise program that includes a combination of postural, flexibility, strength and trunk control exercises. The specific exercise mix is dependent on the individual needs of my clients and I choose what is appropriate after an assessment.
Daily Postural and Flexibility Lumbar Compression Fracture Exercises
Each of these compression fracture exercises can be found in Exercise for Better Bones. I decide the appropriate mix of postural and flexibility exercises based on my assessment of the individual.
- Chest stretch
- Chin tuck
- Arm lengthening or reach back
- Arm pull back
- Shoulder Stabilization
With time I encourage you to progress the chest stretch by lying on your back over a rolled-up blanket. Place the blanket lengthways.
Straighten your arms out at the height of your shoulders (shown in Stronger Bones Stronger Body workout video) to open up your chest wall and reduce the constant forward pull into gravity.
Strength and Trunk Control Lumbar Compression Fracture Exercises
A selection of these compression fracture exercises can be done up to three times per week. I decide the appropriate mix of strength and trunk control exercises based on my assessment of the individual.
- Abdominal activation
- Wall push-ups
- Bridging
- Prone leg lift
- Squats
- Step ups
- Bicep curls
- Horse Stance
- Floor M
- Reverse Fly
Finally, I encourage you to work with a health care professional who can provide soft tissue massage, postural taping, or taping and gentle spinal mobilization.
Exercise Recommendations for Osteoporosis
Exercise is an essential ingredient to bone health. If you have osteoporosis, therapeutic exercise needs to be part of your osteoporosis treatment program.
But what exercises should you do and which ones should you avoid? What exercises build bone and which ones reduce your chance of a fracture? Is Yoga good for your bones? Who should you trust when it comes to exercises for osteoporosis?
A great resource on exercise and osteoporosis is my free, seven day email course called Exercise Recommendations for Osteoporosis. After you provide your email address, you will receive seven consecutive online educational videos on bone health — one lesson each day. You can look at the videos at anytime and as often as you like.

I cover important topics related to osteoporosis exercise including:
- Can exercise reverse osteoporosis?
- Stop the stoop — how to avoid kyphosis and rounded shoulders.
- Key components of an osteoporosis exercise program.
- Key principles of bone building.
- Exercises you should avoid if you have osteoporosis.
- Yoga and osteoporosis — should you practice yoga if you have osteoporosis?
- Core strength and osteoporosis — why is core strength important if you have osteoporosis?
Enter your email address and I will start you on this free course. I do not SPAM or share your email address (or any information) with third parties. You can unsubscribe from my mail list at any time.
Sex With Compression Fractures
My first piece of advice regarding sex with compression fractures is to consult with your physician before engaging I a physical activity such as sex with your partner.
Second, I cover this topic in more detail in my online course, Guide to Living with Compression Fractures.
When Can You Have Sex After a Lumbar Compression Fracture?
There is no need to give up an enjoyable sex life because of a compression fracture. Vertebral compression fractures (VCF) may alter your sex life, but they should certainly not eliminate it.
A compression fracture may make you feel fragile and vulnerable. That is natural.
Have open and honest conversations about these feelings with your partner. It can help you both feel more comfortable with the situation.
Let your partner know how you feel and discuss the support you need. These conversations provide you both with the opportunity to demonstrate love and care for each other.
A vertebral compression fracture can create stress in your relationship. It is important that you keep this in mind and I recommend that many people consider couples therapy during times of stress. You can find a good therapist in your area. For example this is a good source of couples therapy in Toronto.
During the First 8 to 12 weeks of Recovery (May be Longer for Some People)
When you’re in the recovery stage, physical intimacy is best expressed in alternative ways than intercourse. Consider exploring each other through gentle, sensual touch.
After the Healing Phase
Once you have been given the green light by your physician or surgeon to exercise, you can also start exploring intercourse again.
For some with minimal compression(s) in the mid thoracic spine, little may change for you. Lumbar compression fractures will certainly create a bigger impact on the positions you choose and how aggressive you are comfortable being.
Discuss positions you both enjoy as long as you both keep in mind that the partner with a compression fracture has a heightened awareness of their safety.
Symptoms of Compression Fracture
The following are six symptoms of a compression fracture:
- Over the age of 60.
- History of a previous fracture, whether that is a wrist fracture, a toe fracture.
- Have a shorter duration of back pain. Don’t disregard back pain that only lasts a couple of weeks.
- Find that your back pain might not be sharp but a lot of people with vertebral fractures will describe their back pain as crushing in nature.
- Your back pain actually gets better when you lie down.
- Unlike people with sciatica, your back pain most likely will not be, if it’s from a vertebral fracture, will not be going into the leg.
If you have any of these symptoms, especially a combination of these symptoms, you should ask your doctor to assess you for a vertebral fracture.
Many people are not aware that they have a compression fracture. In fact, a recent study (3) states that about 12% of post-menopausal women will have a vertebral fracture but only one third of those will get the attention of a medical professional.
In the video below I identify the symptoms of compression fracture and what you should do if you have a fracture.
Post Menopausal Women and Symptoms of Compression Fracture
A recent study looked at how 12% of people that are post menopausal are going to have a vertebral fracture in their lifetime.
But only one-third — less than 4% of those fractures — are brought to the attention of the doctor and therefore are brought to the attention of the individual.
This is striking, not only am I seeing people with one vertebral fracture or two vertebral fractures, but by the time they come to see me, by the time they’re first diagnosed, they actually have five vertebral fractures.
This is really terrible because it affects their quality of life. Then they become fearful of moving and it’s a vicious circle.
Compression Fractures Can Get Worse
My clients come to see me after they have been diagnosed and no one has told them that their vertebral fractures can get worse (until they meet me). Just because your spine has compressed 70%, it doesn’t mean that it can’t keep compressing.
If you have a compression fracture, it is so important for you to be really meticulous about your alignment because those fractures will get worse. Not only will the actual fractures themselves get worse but you are at a higher risk of fracturing more and more levels. But all is not lost.
Impact of Exercise on Compression Fractures
A recent study (4) shows that a 12 month duration of exercise had a very positive effect for people who had experienced vertebral fractures. The outcome was that after 12 months they had a significant improvement in quality of life. They had an easier outcome of doing their tasks of daily living, their functional mobility was improved and their balance was improved.
If you have been diagnosed with a vertebral fracture do intelligent exercises, avoid all forward flexion, follow the guidelines that I have on my blogs and in Exercise for Better Bones and play it safe and know that you can still improve your quality of life and you can still be stronger.
If you are not sure whether you have a compression fracture but have any of the six symptoms listed above have it investigated.
What is Compression Fracture
I want to talk about a topic that is especially close to my heart: movements that increase your risk for spinal fractures or compression fractures. During this discussion of the movements that cause a fracture we will get into detail on what is a compression fracture.
Compression Fracture Movements
Many new clients come to me for Physical Therapy compression fracture treatment because they receive advice from fitness trainers or books that does not take into account the fact that they have osteoporosis, osteopenia or low bone density. The clients think that they are doing things that are sound and right for them given the fragility of their bones. They are trying their very best.
Unfortunately, there are a lot of movements that they are doing (under the guidance of a fitness instructor or book that is not familiar with osteoporosis) that might be good for the general public but not for individuals with low bone density, osteopenia or osteoporosis. These movements are putting them at risk of a compression fracture.
By the end of this tutorial, you’ll have a good understanding of what movements, be it in yoga, pilates, in an exercise class or movements around the house, that you should modify.
Spine Anatomy: Compression Fracture in Back
In this tutorial, we’re going to look at why the lumbar and thoracic spine is more at risk than other bones in the body of a compression fracture. This would be a good time to review, if you haven’t yet done, the tutorial on understanding bone.
(To follow this tutorial you will have to play the embedded video because I will refer to images and diagrams as I speak through the talk.)
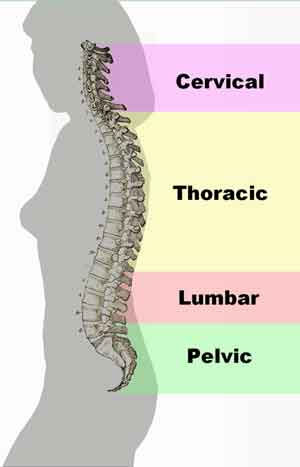
The illustration shows the normal curves in our spine. We have a normal inward curve in our lumbar spine, or our low back, which is referred to as a lordosis. A normal inward curve in our upper spine, which is the cervical lordosis, is at our neck. We have a normal small outer curve in our upper back, referred to as the thoracic spine.
These curves look really pronounced in our illustration. But if you look at somebody with good alignment, you’ll usually see a nice shape to the spine.
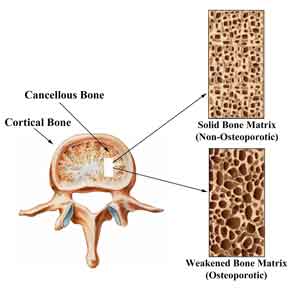
We know from previous tutorials that the vertebral body is composed of a hard outer coating. This hard coating is referred to as cortical bone.
The cortical bone surrounds the trabecular bone in the inside — the softer bone. The trabecular bone is commonly referred to as cancellous or spongy bone.
The illustration to the right shows the cross section of a vertebra of the spine. The cortical bone is the thick non-porous bone at the rim on the cross section of the spine. The trabecular bone is the porous bone in the center of the cross section.

Thoracic Compression Fracture Versus Lumbar Compression Fracture
A compression fracture can happen anywhere along the spine. The incidence of thoracic compression fracture is the highest among all parts of the spine because this area is the one where the postural stoop (or kyphosis) will occur. You could experience a lumbar compression fracture when you have an impact. I had a client who went tobogganing with her grandchildren. As they were going down the snow run they hit a few bumps — enough to cause a lumbar compression fracture and considerable pain.
Flexion Exercise Versus Extension Exercise
In the 1980’s, we weren’t sure whether flexion or extension exercises were a safe thing to give to a woman with osteoporosis or people with back pain. Fortunately there were physicians who studied this issue.
If you who are not familiar with flexion and extension exercises, I have two photos showing each type of exercise.
The first photograph on shows a flexion exercise. Note how our model Pat is rounding her back in order to complete the sit up or crunch exercise. Unfortunately, this exercise is still very popular in exercise classes and used by many personal trainers.

The second photo shows an extension exercise.
Note how our model Aline, in the photo, is performing the Prone M (also referred to as Floor M) exercise by elevating her torso upwards and creating an extension of her back.
I also prepared a video explaining flexion and extension.

In 1984, Dr. Mehrsheed Sinaki at the Mayo Clinic did a study (5) on postmenopausal osteoporotic women that looked at the effects of flexion exercises versus extension exercises.
The mean age or the average age for the women in this study were 49 to 60 years of age.
She broke the study set into four exercise groups:
- First group did extension exercises.
- Second group did flexion exercises.
- Third group did a combination of flexion and extension exercises.
- Fourth group did no exercise at all.
Within a year and a half, if they had back pain or if they were due for a follow-up, members of the study set would report back in. Dr. Sinaki did spinal x-rays and would see whether or not they had sustained fractures of the spine. These were the findings.
Flexion Compression Fracture
Compression fractures occurred at the following rates by group:
| Group | Exercise Class | Fracture Rate |
| 1 | Extension Exercises | 16% |
| 2 | Flexion Exercises | 89% |
| 3 | Extension & Flexion | 59% |
| 4 | No Exercise | 67% |
The study found that fractures occurred at a very high rate, 89%, in the group that had done flexion exercises (group #2), such as sit ups and toe touch exercises.
The group that did no exercise at all (group #4) still had a very high rate of fracturing. The thought behind that is that for a lot of things that we do in life such as picking out the laundry, reaching forward, coughing, sneezing, involves a lot of flexion.
Further, unless we counteract that with some extension exercise, as you see in group #3 where they did some extension and some flexion, you will not reduce your rate of compression fracture.
The group that did just extension exercises (group #1) had a very low rate of fracturing. Sixteen percent in comparison to 90%. This is a substantial difference.
Why Flexion Causes Compression Fractures
Let’s take a closer look at what happens to your spine when you do flexion exercises or perform activities that cause a flexion motion. The image provides a closer look at the actual trabeculae or the cross-bridges within the vertebral body. When we do a lot of flexion motions of the spine, as well as side flexion and extremes of rotation, those motions have been implicated with high forces and can cause excessive stress on the vertebral body.
The weakened trabeculae in osteoporotic bone can’t withstand those excessive forces. As a result, they start to fracture. You can see in this vertebral body that there are large pits. The weakened areas are unable to bear the stress caused by the flexion (wether through exercise, activities of daily living or other sources) with the result being a compression fracture.
The x-ray image of the spine below shows a compression fracture. The white vertebra is compressed. This can cause a loss of height of the vertebrae.
What has happened is that there’s been so many forces that the disc is actually starting to push through the vertebrae. The vertebrae itself is actually quite a bit shorter in stature than the vertebrae above and below it. It has just compressed in on itself.

How to Reduce Kyphosis
If we want to stop the progression of forward flexing of the spine (kyphosis) that occurs because of the repeated wedge fracturing like we see in the image to the right, we need to do this at a stage ideally where the individual has not yet fractured. This is also known as a Dowager’s Hump, buffalo hump, or neck hump.
We prefer to work with them when they are still able to hold their ear over their shoulder and their shoulder over their hip in nice alignment.
Exercise and movements during the day that put our spine in flexion are implicated. We need to make sure that when you are moving, that you have the best alignment possible.
In the video, you will see Pat, one of my clients, demonstrating how to garden safely.
In the photo, Pat is bending forward in an unsafe manner. She is putting a lot of force on her spine, especially in her mid back, through this position. She is lifting a heavy bag in a flexed position. This movement could cause a compression fracture.

If she took the time to get down and kneel, as she is demonstrating in the second photo, she will maintain a nice postural alignment.
The bending is happening in the knee and hip as opposed to the spine. That’s much safer on the spine. The loading through trabeculae and the whole vertebral body is much more even and safe.

Exercises and Movements That Increase Risk of Compression Fracture
Studies have shown that exercises that involve flexion increase your chance of spinal fracture. They have also demonstrated that exercises that involve the combination of flexion and rotation increase fracture risk even more than flexion exercises only.
Daily activities can be problematic. I will often see women carry heavy purses and they go to sit down and they’ll rotate and drop their purse to the side. Movements like create a very compressive load and put your spine at risk of a compression fracture.
Movement Strategies to Avoid a Compression Fracture
Here are several movement strategies that will reduce your risk of a compression fracture.
Follow an exercise program designed for people with osteoporosis. Exercise for Better Bones is an osteoporosis exercise program that provides exercise programs for people at different fracture risk and activity levels.
Make sure you follow good movement patterns during your activities of daily living (ADL). There is a comprehensive guide on safe movement included with Exercise for Better Bones.
Yoga and pilate moves need to be practiced with caution and should be practiced under the supervision of instructors who are well trained in the precautions that need to be carried out for individuals with osteoporosis and low-bone density. If you want more information or have an instructor who wants more information, consider Yoga for Better Bones. It provides details on Yoga poses you should modify or avoid.
Avoid exercises that put you in flexion. Stay clear of exercises that involve flexion and rotation. I wrote a detailed post on osteoporosis exercises to avoid.
Types of Vertebral Compression Fractures
Not every vertebral compression fracture is alike. Just as we are all unique in our makeup, the same applies to compressions that can occur in the spine. The most significant risk factor for obtaining a vertebral compression fracture is having osteoporosis.
Compression fractures may be classified based on the portion of the vertebral body that is affected. (1) They are generally classified when at least 20% of the height of the affected portion is lost.
Wedge Vertebral Compression Fracture
The wedge vertebral compression fracture takes its name from the shape that is created as the front or anterior of the vertebral body is affected.
Wedge compressions are most commonly seen in the mid back, around the level of the lower angle of the shoulder blades.
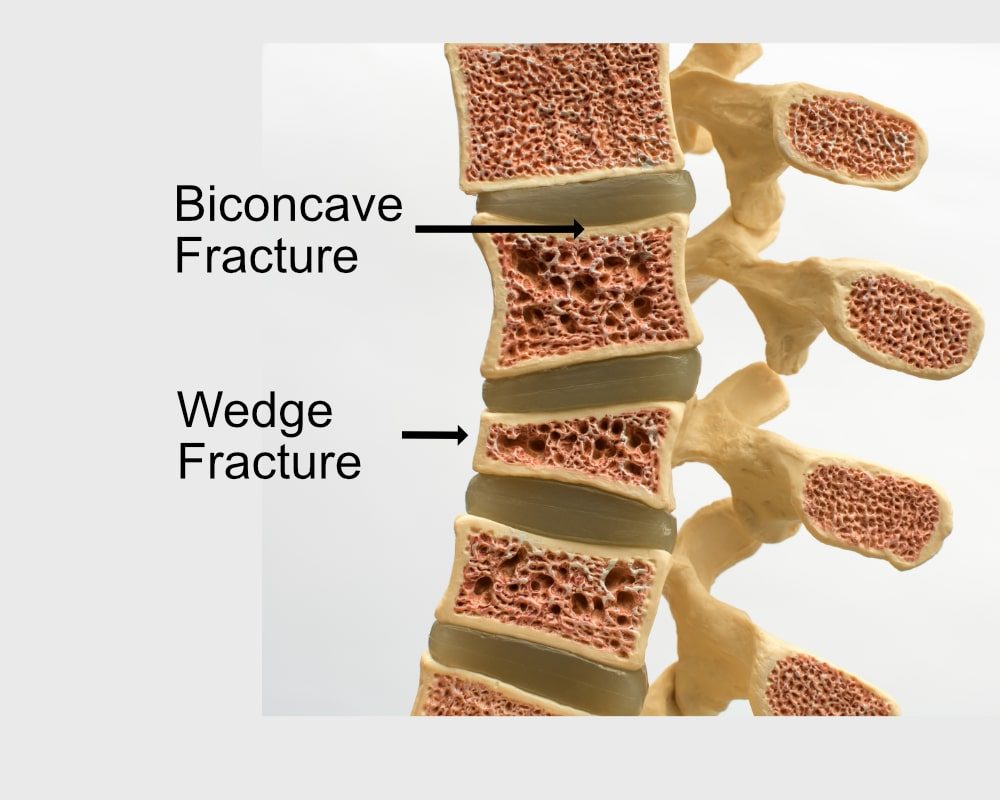
Biconcave Vertebral Compression Fracture
The biconcave vertebral compression fracture, like the wedge fracture can have different levels of compression. With a biconcave vertebral compression fracture the middle of the vertebra collapses.
With biconcave fractures the top of the vertebral body takes on what looks like a smile while the bottom of the vertebral body takes on a grin.
In the next lessons I cover in more detail what types of movements have been shown to increase the risk of both wedge and biconcave vertebral compression fractures.
Crush Vertebral Compression Fracture
A crush vertebral compression fracture is the least common type of vertebral compression fracture. In crush fracture the posterior portion of the vertebral body collapses.
The last type of compression fracture is classified as complex.
How Do I Strengthen my Back After a Compression Fracture?
In order to strengthen your back (and improve your posture) after a vertebral compression fracture, I highly recommend that you start with the postural exercises in Exercise for Better Bones and then build from there to the Beginner strength exercises. After that, continue through to the Active strength exercises.
All of those exercises are incredibly safe and progressive.
Take it one day at a time, one exercise at a time, and progress at a pace that works for you.
Weight Lifting After Compression Fracture?
Yes, absolutely.
How much weight can you safely lift?
I don’t know.
It depends on your body, how strong you were, the quality of your bone, and your form when you exercise.
It is always best to start slowly and gradually with baby steps. Start at the beginner level, gradually work your way up, see what your body allows you to do, and maximize the weight that you can lift safely.
Can I Wear or Use a Weighted Vest After a Compression Fracture?
Weighted vesta are a popular exercise device for many people with osteoporosis but should you wear one if you have a compression fracture? I answer that question in this video:
Can You Drive with a Compression Fracture?
If you find that you have no pain sitting or doing shoulder checks, then there’s no reason that you can’t drive.
However, I have a number of clients who took several months, even some as long as nine months, to be comfortable driving. This was due to the fact that they would place their hands down by their side to brace themselves when the car went over a little pothole or bumpy spaces in the road.
If they were driving, they didn’t feel they had the control of both their body and the car at the same time.
So it’s a personal decision that you’re going to have to make to keep you safe and feeling well.
Is a Heating Pad Good for a Compression Fracture?
Yes, it is.
In the early phases of your vertebral fracture, there will be some inflammation around the vertebral body itself, but the heat pad can be applied away from the vertebral bodies and to all the back muscles on either side of the vertebrae. The heat helps the muscles to relax.
As time goes on, your spine has to work a little harder if you have compressions because the forces in the spine have changed.
The heating pad is nice when you’re taking your break before bed or taking siesta in the afternoon, for example, to bring some blood flow to the muscles and give them a little break throughout the day.
As mentioned earlier in this post, Brenda uses a heating pad a lot. When she starts to feel achy, she sits down for 15 minutes and puts it on. It helps take the ache away. When she does her stretching exercises, she has it underneath her as well.
Best way to Sleep with Compression Fractures
Here is my recommended osteoporosis sleeping position for people with compression fractures. This is likely the best sleeping position for osteoporosis of the spine:
- If you wear pyjamas to bed, choose silky material to help reduce friction and make moving in your bed easier.
- ‘Log roll’ when turning in bed. Keep your knees bent, roll your shoulders and knees simultaneously.
- Use extra pillows to ensure a supportive sleeping position.
- Use a heating pad to help your muscles relax.
- Consider wearing a waist belt to support the space between your lower ribs and pelvis.
- Use a pillow under your knees/legs when sleeping on your back.
- Keep your head pillow as low as you comfortably can when on your back.
- Use a pillow between your knees and ankles when sleeping on your side.
- If you are a side sleeper, make your head pillow wide enough that it supports your head in a neutral position (i.e. that your chin is in at the level of the middle of your breastbone).
- Consider sleeping in your own bed so that you do not have the worry of your partner’s movements jarring your back.
- Avoid sleeping in a recliner. Get as flat as you comfortably can so as to take weight off your compressed vertebra.
- Avoid a water bed.
- Avoid a memory foam mattress if you keep your room cooler than 65 degrees Fahrenheit at night (because they get too stiff).
- Medium-firm mattress is often recommended but you have to find the one that is right for you. Make sure you spend at least 10 minutes lying on one at the shop. Wear the same thickness of clothes you would at night.
To learn more about how to get a good night’s sleep if you have a compression fracture, visit my page dedicated to better sleep.
How to Get Out of Bed With a Compression Fracture
Here are my recommendations for patients with compression fractures who want to know how to get out of bed with a compression fracture:
- Use your pelvic floor and deep abdominal muscles to brace your back when getting in and out of bed.
- To get out of bed, ‘log roll’ onto your shoulder and then push yourself up with your hands until you are in a sitting position.
- To get in bed, get in a sitting position. Carefully tilt down, lower yourself with your hands and roll onto your shoulder until you are lying flat on your side.
Compression Fracture and Back Pain
A comprehensive study published in the Journal of Bone and Mineral Density in September 2017 (7) identified a relationship between the incidence of compression fracture and back pain.
The research team examined data from 4,396 men over the age of 65. The men had enrolled in the Osteoporotic Fractures in Men study between 2000 and 2002. The key findings and conclusions were:
- Only 25% of new vertebral fractures are diagnosed by their physician.
- Approximately 60% of older men with small osteoporosis-related compression fractures reported new or worsening back pain.
- The percentage of men in the study reporting back pain with undiagnosed compression fractures (70%) exceeded those without compression fractures by 11 percentage points (59%).
- 93% of the men who had their fractures diagnosed during the study reported back pain.
- Prevention the compression fractures could have reduced the onset of back pain and further disability in the study group.
The study’s main author, Dr. Howard Fink, concluded: “Back pain is the most common symptom (of compression fractures).” The study results are similar to findings in elderly women.
Recall that Brenda experienced severe back pain during her trip to Africa — likely brought on by a compression fracture. If you experience back pain, consult your physician and specifically ask if she can determine if the cause is a compression fracture.
Exercise Recommendations for Osteoporosis
Exercise is an essential ingredient to bone health. If you have osteoporosis, therapeutic exercise needs to be part of your osteoporosis treatment program.
But what exercises should you do and which ones should you avoid? What exercises build bone and which ones reduce your chance of a fracture? Is Yoga good for your bones? Who should you trust when it comes to exercises for osteoporosis?
A great resource on exercise and osteoporosis is my free, seven day email course called Exercise Recommendations for Osteoporosis. After you provide your email address, you will receive seven consecutive online educational videos on bone health — one lesson each day. You can look at the videos at anytime and as often as you like.

I cover important topics related to osteoporosis exercise including:
- Can exercise reverse osteoporosis?
- Stop the stoop — how to avoid kyphosis and rounded shoulders.
- Key components of an osteoporosis exercise program.
- Key principles of bone building.
- Exercises you should avoid if you have osteoporosis.
- Yoga and osteoporosis — should you practice yoga if you have osteoporosis?
- Core strength and osteoporosis — why is core strength important if you have osteoporosis?
Enter your email address and I will start you on this free course. I do not SPAM or share your email address (or any information) with third parties. You can unsubscribe from my mail list at any time.
Conclusion: How to Treat a Compression Fracture
We have covered a wide range of issues related to compression fractures. We learned why your spine is at risk of a compression fracture and about physical therapy compression fracture treatment. Brenda’s story shows that every person’s experience with compression fracture is going to be different.
We identified six symptoms that you might have a compression fracture. I have quite a few clients that have compression fractures and do not even know they ever had them. I’ll ask them to get x-rays because I’m trying to convince them to move safer. Some clients might have had a bit of back pain that goes away after six to eight weeks. They’re the lucky ones. Their compressions fracture may not always stay like that.
Brenda’s experience shows that you should find a health practitioner that you trust and has knowledge in treatment of osteoporosis and compression fractures.
There are many things that you can do to make your life with a compression fracture. We covered these in this blog post.
Safe compression fracture exercises and safe movement are critical to reducing your risk of another compression fracture.
I hope that this blog does help make the life of listeners a little bit easier out there, and if anybody wants to add their comments at the end the blog, feel free to do so.
Margaret Martin
More on Compression Fracture
References
- Mokhtarzadeh H, Anderson DE. The Role of Trunk Musculature in Osteoporotic Vertebral Fractures: Implications for Prediction, Prevention, and Management. Curr Osteoporos Rep. 2016 Apr 4. [Epub ahead of print]
- Kim L Bennell, Bernadette Matthews, Alison Greig, Andrew Briggs, Anne Keppy, Margaret Sherburn, Judy Larsen, John Wark. Effects of an Exercise and Manual Therapy Program on Physical Impairments, Function and Quality-of-life in People with Osteoporotic Vertebral Fracture: A Randomized, Single-blind Controlled Pilot Trial. BMC Musculoskeletal Disorders. Posted 03/19/2010
- Clark E.M., Gooberman-Hill R, Peters TJ. Using self-reports of pain and other variables to distinguish between older women with back pain due to vertebral fractures and those with back pain due to degenerative changes. Osteoporosis International. April 2016, Volume 27, Issue 4, pp 1459-1467
- EvstigneevaL et al. Effect of twelve-month physical exercise program on patients with osteoporotic vertebral fractures: a randomized, controlled trial. Osteoporos Int. 2016 Mar 16. [Epub ahead of print]
- Sinaki M, Mikkelsen BA, Postmenopausal spinal osteoporosis: flexion versus extension exercises, Arch Phys Med Rehabil. 1984 Oct; 65(1): 593-6
- Association of Incident, Clinically Undiagnosed Radiographic Vertebral Fractures With Follow‐Up Back Pain Symptoms in Older Men: the Osteoporotic Fractures in Men (MrOS) Study, Howard A Fink et al, Journal of Bone and Mineral Density, September 7, 2017

Comments